Can Acupuncture Improve Digestive Issues? A Functional & Traditional Chinese Medicine Perspective
How Acupuncture Supports Gut Motility, Nervous System Regulation, and Digestive Healing
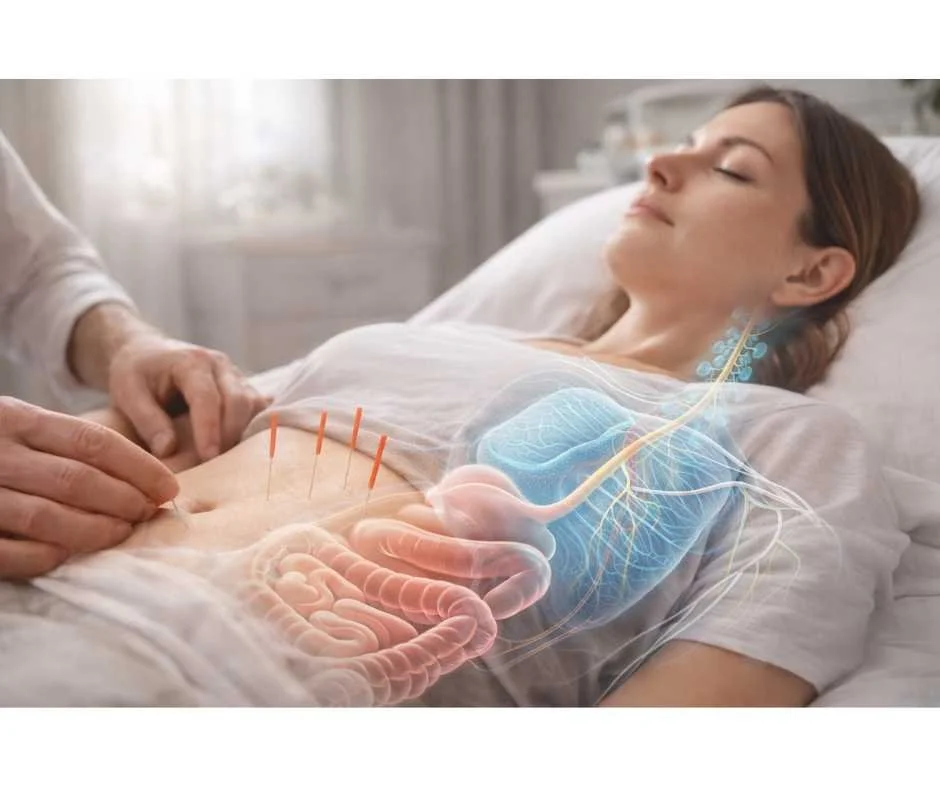
Acupuncture for digestive health sits at the intersection of ancient medical wisdom and modern neuro-gastroenterology. The digestive system is not simply a mechanical tube—it is a highly regulated, neurologically driven network that depends on coordinated motility, intact vagal tone, appropriate inflammatory signaling, and adequate blood flow.
Acupuncture supports digestive function by addressing the regulatory systems that commonly underlie chronic digestive issues such as bloating, IBS, reflux, and irregular bowel habits.
When this coordination breaks down, symptoms such as bloating, reflux, constipation, diarrhea, abdominal pain, or irregular bowel habits can emerge. While conventional medicine often focuses on symptom suppression, acupuncture approaches digestive dysfunction through regulation—of the nervous system, organ communication, and systemic balance.
In both Traditional Chinese Medicine (TCM) and functional medicine, digestion is viewed as foundational to overall health. When digestion suffers, downstream systems—including immune, hormonal, and metabolic function—are inevitably affected.
This article explores how acupuncture supports digestive healing, how it interfaces with the autonomic nervous system, and why it is increasingly used alongside functional medicine strategies for gut restoration.
Can Acupuncture Help With Digestive Issues?
Yes. Acupuncture is widely used as a complementary therapy for digestive conditions and is supported by a growing body of clinical research. Evidence suggests acupuncture can help regulate the autonomic nervous system, reduce visceral hypersensitivity, modulate inflammation, and improve gut motility—key mechanisms involved in functional and inflammatory digestive disorders. (1)
Rather than acting as a stand-alone “cure,” acupuncture works best as part of a comprehensive digestive care plan, particularly for patients with chronic, stress-responsive, or functional gut conditions.
The Connection Between Acupuncture and Digestive Health
In Traditional Chinese Medicine, digestive health depends on the smooth flow of Qi through organ systems—particularly the Spleen, Stomach, Liver, and Intestines. Disruptions in this flow may manifest as bloating, cramping, reflux, loose stools, or constipation. (2)
From a modern physiological perspective, acupuncture influences digestion primarily through:
Regulation of the autonomic nervous system
Improved vagal tone and parasympathetic signaling
Reduced sympathetic overdrive (“fight or flight”)
Enhanced visceral blood flow
Modulation of inflammatory and pain pathway
Because the gut is directly innervated by the nervous system, therapies that calm and regulate neural signaling can dramatically affect digestive function.
This is why acupuncture is often particularly effective for stress-sensitive digestive disorders such as IBS, functional dyspepsia, and reflux patterns driven by nervous system dysregulation.
Common Digestive Issues Addressed By Acupuncture
In clinical practice, digestive symptoms rarely show up in isolation. Patients often describe years of bloating, reflux, unpredictable bowel habits, or abdominal discomfort that waxes and wanes with stress, diet, or life demands. Research supports what we see in the clinic every day—acupuncture can be a valuable supportive therapy for a range of digestive conditions by helping regulate the nervous system, calm inflammation, and restore digestive rhythm. (3,4)
Irritable Bowel Syndrome (IBS)
Acupuncture may help reduce bloating, abdominal pain, and alternating bowel habits by calming visceral hypersensitivity and regulating gut motility.
IBS is a functional digestive disorder strongly influenced by nervous system dysregulation, gut-brain signaling, microbial imbalance, and stress physiology.
Functional Dyspepsia (Indigestion)
By supporting gastric emptying and nervous system balance, acupuncture may reduce post-meal discomfort, fullness, and upper abdominal pain.
Gastroesophageal Reflux Disease (GERD)
Acupuncture may improve reflux patterns driven by autonomic dysfunction and impaired motility rather than excess stomach acid.
This distinction is critical, as reflux is frequently caused by low stomach acid, delayed gastric emptying, and nervous system dysregulation—not overproduction of acid.
Ulcerative Colitis
Acupuncture may support symptom relief by reducing inflammation, modulating immune signaling, and improving stress resilience alongside medical care.
Crohn’s Disease
While not a primary treatment, acupuncture may help reduce pain, diarrhea, and stress-related symptom flares as part of an integrative approach.
Inflammatory bowel diseases involve immune-driven inflammation, gut barrier disruption, and microbiome imbalance, requiring an integrative approach that supports both immune regulation and digestive healing.
How Acupuncture Supports Digestive Function
Acupuncture does not support digestion through a single mechanism. Instead, it works across multiple physiological systems that govern how the gastrointestinal tract moves, esponds to inflammation, maintains coordinated motility, and adapts to physiologic stress. By influencing these interconnected pathways, acupuncture helps restore coordination and resilience within the digestive process rather than simply suppressing symptoms.
→ Acupuncture & Nervous System Regulation
Regulating Gut Motility
One of acupuncture’s most clinically relevant effects is its ability to regulate gastrointestinal motility. By influencing autonomic nervous system signaling, acupuncture can help normalize peristalsis—supporting both sluggish digestion and hyperactive bowel patterns. (5)
This nervous-system-driven regulation improves coordination within the digestive tract, allowing for more efficient nutrient absorption and waste elimination.
Reducing Gastrointestinal Inflammation
Chronic, low-grade inflammation is one of the most common—and most overlooked—drivers of persistent digestive symptoms. For many patients, inflammation is not limited to a single diagnosis like IBD, but shows up as ongoing gut irritation, food reactivity, visceral pain, and impaired gut barrier function.
Acupuncture influences inflammation through several interconnected pathways. By modulating neuroimmune signaling, acupuncture can reduce the release of pro-inflammatory cytokines while supporting regulatory immune responses that help calm intestinal irritation. (6) This is particularly relevant for patients with IBS, post-infectious gut symptoms, dysbiosis, or autoimmune-related digestive conditions.
Clinically, reducing inflammation often translates to less abdominal pain, fewer flare-ups, improved stool consistency, and greater tolerance to dietary changes. Rather than targeting inflammation in isolation, acupuncture helps shift the body out of a chronic inflammatory state by improving nervous system balance, circulation, and immune communication—creating a more stable internal environment for true gut healing.
Supporting Hormonal And Endocrine Balance
Digestion is deeply intertwined with hormonal signaling. Gastrointestinal motility, enzyme secretion, bile flow, appetite regulation, and blood sugar control are all influenced by hormones that respond to stress, circadian rhythm, and metabolic health.
Acupuncture’s effects on the endocrine system may help restore balance in patients whose digestive symptoms worsen alongside hormonal dysregulation, adrenal stress, or blood sugar instability. (7) This is especially common in individuals experiencing chronic stress, perimenopause, metabolic dysfunction, or overtraining—where digestive complaints often coexist with fatigue, sleep disruption, and mood changes.
By supporting neuroendocrine regulation, acupuncture can help normalize digestive timing, reduce stress-related appetite changes, and improve overall metabolic signaling. This systemic support is one reason acupuncture can be particularly effective when digestive symptoms do not respond to diet changes alone.
Digestive symptoms that worsen with stress, blood sugar swings, menstrual cycle changes, fatigue, or metabolic strain often reflect deeper hormonal imbalances. In these cases, identifying cortisol patterns, sex hormone metabolism, thyroid signaling, and insulin dynamics is essential for creating an effective, individualized care plan.
Thyroid signaling is a major regulator of digestive motility, stomach acid production, and intestinal transit time, and dysfunction can quietly drive bloating, constipation, reflux, or diarrhea—even in patients who are eating “clean” and taking supplements.
Managing Stress
A stressed mind often manifests as a stressed gut. Digestive symptoms such as bloating, cramping, reflux, or irregular bowel habits commonly flare during periods of emotional strain, cognitive overload, or chronic pressure. For many patients, symptoms are less about food alone and more about how the body responds to stress.
Acupuncture helps by improving the body’s ability to tolerate and recover from stress exposure. Clinically, this may translate into more predictable digestion, reduced gut tension, fewer stress-triggered flares, and improved symptom resilience over time. Rather than suppressing symptoms, acupuncture supports the regulatory capacity that allows digestion to function more consistently even when stressors are present. (8)
This gut–mind relationship underscores why addressing stress physiology is often essential for meaningful, long-term digestive improvement.
Key Acupuncture Points For Digestive Health
In clinical practice, acupuncture point selection is never generic or protocol-driven. Digestive symptoms that appear similar—such as bloating, reflux, constipation, or diarrhea—may arise from very different underlying patterns involving nervous system dysregulation, impaired motility, inflammation, or stress physiology. While each treatment is individualized, certain acupuncture points are commonly used because of their reliable effects on digestive function, nervous system balance, and organ communication. (9)
Zusanli (ST36)
Often referred to as the “Leg Three Miles,” Zusanli is one of the most important points for digestive health. It supports stomach and spleen function, enhances nutrient absorption, and helps regulate bowel motility. Clinically, it is frequently used for bloating, nausea, poor appetite, fatigue, and generalized digestive weakness.
Tianshu (ST25)
Located on the abdomen, Tianshu is a key point for regulating intestinal function. It is commonly used for constipation, diarrhea, abdominal cramping, and IBS-related symptoms by helping normalize peristalsis and reduce intestinal stagnation.
Sanyinjiao (SP6)
Sanyinjiao harmonizes the spleen, liver, and kidney systems and plays an important role in both digestive and hormonal balance. It is often used for bloating, loose stools, digestive sluggishness, and stress-related gut symptoms, particularly in patients whose digestion fluctuates with hormonal changes.
Neiguan (PC6)
Neiguan is strongly associated with calming the nervous system and regulating the upper digestive tract. It is frequently used for nausea, reflux, early satiety, and stress-induced digestive discomfort, especially when symptoms worsen with anxiety or emotional strain.
Qihai (CV6)
Located on the lower abdomen, Qihai supports overall digestive vitality and energy. It is commonly used in cases of weak digestion, chronic fatigue, and poor resilience, helping strengthen the body’s ability to process and assimilate nutrients.
Hegu (LI4)
Hegu plays a key role in regulating pain, stress responses, and digestive discomfort. It is often included in treatments for abdominal pain, tension-related digestive symptoms, and stress-driven gut dysfunction.
Taichong (LV3)
Taichong helps regulate liver Qi and relieve stress-related stagnation that can impair digestion. It is commonly used when digestive symptoms are closely tied to emotional stress, tension, or irregular eating patterns.
Together, these points illustrate how acupuncture approaches digestion as a systems-based process—supporting motility, calming the nervous system, improving circulation, and restoring balance rather than targeting isolated symptoms.
A Holistic Approach To Digestive Health
Sustainable digestive healing rarely comes from a single intervention. The gut is influenced by a complex interplay of nervous system signaling, diet, inflammation, hormonal balance, stress load, and daily habits. Acupuncture works most effectively when it is part of a broader, systems-based approach that supports these interconnected pathways rather than addressing symptoms in isolation.
When acupuncture is combined with targeted nutrition, stress regulation, and appropriate movement, it can help create the physiological conditions needed for digestion to normalize—improving motility, reducing reactivity, and supporting long-term resilience of the gut.
In clinical practice, a holistic digestive plan often includes:
Nutrition
Nutrition is foundational to digestive healing, but there is no universal “perfect diet” for gut health. What supports one person’s digestion may aggravate another’s, depending on factors such as enzyme output, microbiome balance, motility, inflammation, and nervous system tone. Rather than following generic dietary rules, nutrition is tailored to the individual’s digestive capacity, symptom pattern, and underlying imbalances.
In clinical practice, this may involve adjusting meal timing, food quality, macronutrient balance, or temporarily removing foods that increase fermentation, gas, or gut irritation while healing is underway. For patients with bloating, IBS-type symptoms, or suspected dysbiosis, structured elimination approaches can be particularly helpful when used strategically and short term.
Timing And Consistency
Digestive function is highly responsive to rhythm. Irregular eating patterns, chronic snacking, late-night meals, or eating under stress can disrupt digestive signaling and impair motility. Acupuncture can be timed strategically during periods of high stress, digestive flares, or transitions in care to reinforce nervous system regulation and improve the body’s responsiveness to meals.
Establishing consistency—around meal timing, sleep, and treatment schedules—helps stabilize gut-brain communication and supports more predictable digestion over time.
Stress Regulation
Chronic stress is one of the most powerful—and often underestimated—suppressors of digestion. When stress is persistent, digestive function becomes less predictable: motility slows or fluctuates, digestive secretions become less efficient, and inflammatory patterns are more likely to persist. Many patients notice that symptoms worsen during periods of emotional strain, disrupted sleep, or sustained mental load, even when diet remains unchanged.
Pairing acupuncture with intentional stress-regulation practices—such as breathwork, mindfulness, or gentle nervous system retraining—helps restore consistency and resilience within the digestive process. Clinically, this often allows nutritional and supplement strategies to become more effective, because the body is no longer operating in a state that suppresses digestion. For many individuals, addressing stress regulation is the missing link that enables other interventions to finally work.
Movement And Circulation
Appropriate physical activity plays an important role in digestive health by supporting gut motility, lymphatic flow, and metabolic regulation. Movement helps stimulate intestinal transit and improves circulation to the digestive organs, while excessive or poorly timed exercise can worsen symptoms by overstimulating the nervous system.
When combined thoughtfully with acupuncture, movement reinforces digestive rhythm without creating additional stress on the system. The goal is not intensity, but consistency and appropriateness for the individual’s current state of health.
By integrating acupuncture with personalized nutrition, stress regulation, and supportive lifestyle strategies, digestive care becomes proactive rather than reactive. This approach addresses root causes, restores physiological balance, and supports the body’s natural capacity to heal—rather than chasing symptoms as they arise.
→ Gut Health & Digestive Restoration
Embark On Your Journey To Digestive Wellness
Digestive symptoms are often the body’s way of signaling deeper imbalance—whether rooted in nervous system dysregulation, inflammation, hormonal shifts, or chronic stress. Acupuncture offers a time-honored yet clinically relevant approach to restoring digestive function by working with the body’s regulatory systems rather than overriding them.
If you’re struggling with chronic bloating, reflux, IBS, inflammatory bowel conditions, or stress-driven digestive symptoms, acupuncture may play a valuable role in restoring balance and improving gut function.
At Denver Sports & Holistic Medicine, we take an integrative, root-cause approach to digestive health—combining acupuncture, nervous system regulation, functional medicine, and personalized care strategies based on your unique physiology.
If you’re ready to move beyond symptom management and address digestion at the nervous system and systems-biology level, we invite you to request a free 15-minute consultation wtih Dr. Martina Sturm to explore whether acupuncture and integrative digestive care are the right fit for you.
Frequently Asked Questions About Acupuncture For Digestive Health
Can Acupuncture Help With IBS
Acupuncture may help reduce IBS symptoms by supporting nervous system regulation, easing visceral hypersensitivity, and improving motility patterns that contribute to bloating, cramping, constipation, or diarrhea. It is often most effective when combined with nutrition and root-cause evaluation.
Can Acupuncture Help With GERD Or Acid Reflux
Acupuncture may support reflux symptoms by improving vagal tone, reducing stress-driven digestive dysfunction, and supporting gastric motility. For many patients, reflux is more related to impaired digestion and pressure patterns than excess acid, so a systems-based approach tends to be most effective.
How Many Acupuncture Sessions Are Needed For Digestive Issues
Some people notice changes within a few sessions, while chronic digestive symptoms typically require a structured plan over several weeks. Frequency depends on symptom severity, stress load, and whether there are underlying contributors like dysbiosis, inflammation, or hormonal imbalance.
What Digestive Symptoms Respond Best To Acupuncture
Acupuncture is commonly used to support bloating, nausea, constipation, diarrhea, abdominal discomfort, reflux patterns, stress-related digestive symptoms, and functional digestive issues where testing does not show a single obvious cause.
Does Acupuncture Reduce Inflammation In The Gut
Research suggests acupuncture can influence inflammatory signaling and neuroimmune pathways. Clinically, this may translate to reduced abdominal pain, less reactivity, and improved gut comfort, especially when paired with dietary and lifestyle strategies.
Can Acupuncture Help With Stress-Related Digestive Problems
Yes. Stress is a major driver of digestive symptoms because it shifts the body out of rest-and-digest physiology. Acupuncture can help activate parasympathetic function, reduce stress hormone output, and improve digestion that is disrupted by chronic tension or anxiety.
Can I Do Acupuncture If I Have IBD
Acupuncture is not a replacement for medical management of IBD, but it may be used as supportive care to help regulate stress physiology, reduce pain, and improve quality of life. Treatment should be coordinated with your broader care plan.
Should I Combine Acupuncture With Functional Lab Testing
If symptoms are persistent, recurring, or complex, pairing acupuncture with functional testing can improve precision. Testing may help identify drivers such as dysbiosis, nutrient deficiencies, inflammation patterns, or hormone and stress physiology that influence digestion.
Still Have Questions?
If the topics above reflect ongoing symptoms or unanswered concerns, a brief conversation can help clarify whether a root-cause approach is appropriate.
Resources
Autonomic Neuroscience – Acupuncture and regulation of the autonomic nervous system in gastrointestinal function
National Center for Complementary and Integrative Health – Acupuncture: In Depth
World Journal of Gastroenterology – Acupuncture for irritable bowel syndrome: systematic review and meta-analysis
Neurogastroenterology & Motility – Clinical evidence of acupuncture in functional gastrointestinal disorders
American Journal of Physiology – Gastrointestinal and Liver Physiology – Effects of acupuncture on gastrointestinal motility and visceral sensitivity
Brain, Behavior, and Immunity – Anti-inflammatory mechanisms of acupuncture in gastrointestinal disease
Psychoneuroendocrinology – Neuroendocrine regulation and hormonal effects of acupuncture
Neurogastroenterology & Motility – Stress, autonomic nervous system regulation, and digestive function
Evidence-Based Complementary and Alternative Medicine – Acupuncture point specificity and gastrointestinal outcomes