Is Gluten Making Your Gut Leaky? 5 Signs to Watch For and How to Heal Naturally
Discover how gluten contributes to intestinal permeability, the key warning signs to watch for, and proven strategies to support gut repair
If eating bread, pasta, or other gluten-containing foods leaves you bloated, fatigued, or mentally foggy, the issue may go deeper than simple food intolerance. For many people, gluten contributes to intestinal permeability, commonly referred to as leaky gut—a condition in which the gut’s protective barrier becomes compromised and allows inflammatory triggers to pass into the bloodstream.
The gut lining is designed to be highly selective. It absorbs nutrients while keeping harmful substances out. When this barrier is disrupted, immune activation and inflammation can follow, often showing up as digestive symptoms, energy crashes, skin issues, joint pain, or worsening autoimmune flares. Gluten is a well-recognized trigger for this process in susceptible individuals because it can interfere with the tight junctions that hold the gut lining together.
What makes this connection easy to miss is that symptoms are not always immediate or purely digestive. Some people tolerate gluten for years before problems surface, while others notice subtle, persistent symptoms that never fully resolve—even after switching to a gluten-free diet. This is often a sign that gut damage has already occurred and needs targeted support to heal.
In this article, we’ll cover five key signs that gluten may be contributing to a leaky gut and outline practical, natural strategies to help restore gut integrity. Understanding this connection is a critical step toward moving beyond symptom management and supporting long-term digestive and immune health.
What Is Leaky Gut Syndrome? A Clear, Clinical Explanation
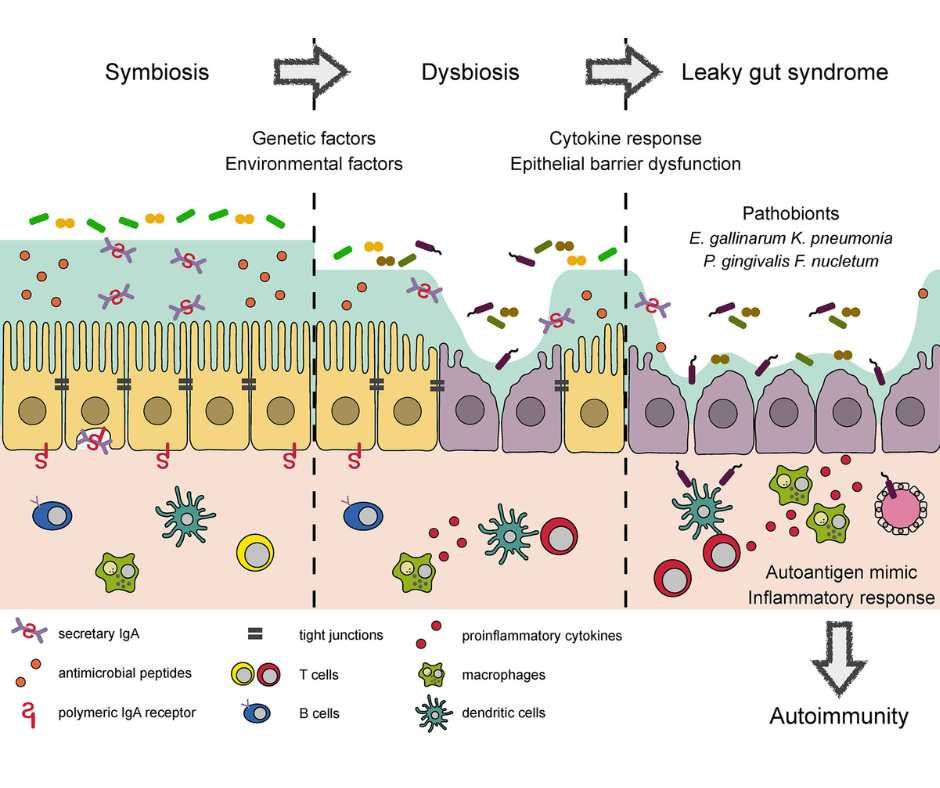
Leaky gut refers to increased intestinal permeability, a state in which the protective lining of the small intestine becomes compromised. Under healthy conditions, this lining acts as a highly selective barrier—allowing nutrients to pass into the bloodstream while keeping bacteria, toxins, and partially digested food particles contained within the gut.
This barrier is maintained by structures called tight junctions, which hold intestinal cells closely together. When these tight junctions are functioning properly, they regulate what can and cannot pass through. Problems arise when these junctions loosen or become dysregulated.
When intestinal permeability increases, unwanted substances can cross the gut barrier and enter circulation. The immune system interprets these particles as threats, triggering inflammation. Over time, this ongoing immune activation can contribute not only to digestive symptoms, but also to systemic issues affecting the skin, joints, brain, and immune system as a whole. (1)
Increased intestinal permeability has been associated with a wide range of chronic conditions, including inflammatory bowel disease, autoimmune disorders, metabolic dysfunction, and cardiovascular disease. This is why leaky gut is not just a digestive concern—it is a whole-body issue.
Understanding leaky gut helps explain why symptoms can be widespread and why simply treating individual complaints often falls short. True healing requires restoring the integrity of the gut barrier itself, calming immune activation, and addressing the factors that caused the breakdown in the first place.
→ Gut Health & Digestive Restoration
→ Functional & Integrative Medicine
How Gluten Can Worsen Intestinal Permeability
Gluten can be a significant driver of leaky gut because of how it interacts with the proteins that regulate the intestinal barrier. One of the key players in this process is zonulin, a signaling molecule that controls the opening and closing of tight junctions between intestinal cells. (2)
In susceptible individuals, gluten stimulates the release of zonulin, which causes tight junctions to loosen more than they should. When this happens repeatedly, the gut barrier becomes more permeable, allowing inflammatory particles to cross into the bloodstream and activate the immune system. Over time, this ongoing exposure can perpetuate inflammation and prevent the gut lining from fully repairing itself.
Gluten rarely acts alone. Several common factors can compound its effects and further weaken the gut barrier, including:
Chronic stress, which alters gut motility, blood flow, and immune signaling
Glyphosate exposure from conventionally grown wheat and other crops, which can disrupt the microbiome and impair gut lining integrity (5)
Alcohol consumption, which increases permeability and inflammatory signaling
Medications such as NSAIDs, antibiotics, and hormonal birth control, all of which are known to affect gut barrier function
Nutrient deficiencies, particularly vitamin D, zinc, and magnesium, which are essential for maintaining tight junction integrity
When these stressors overlap, even moderate gluten exposure can become enough to push the gut past its ability to maintain a healthy barrier. This helps explain why some people tolerate gluten for years before symptoms appear, and why reactions often worsen during periods of high stress or illness.
Addressing gluten-related leaky gut therefore requires more than removing gluten alone. Identifying and reducing these additional stressors is a critical part of restoring gut resilience and preventing ongoing permeability.
→ Gut Health & Digestive Restoration
→ Detoxification & Environmental Medicine
Why Gluten Affects Everyone Differently
Not everyone reacts to gluten in the same way. Some people develop clear digestive symptoms, others experience fatigue, brain fog, joint pain, or autoimmune flares, and some appear to tolerate gluten for years before problems emerge. This variability is not random—it reflects differences in gut health, immune regulation, genetics, and environmental exposure. (3)(4)
Several factors influence how gluten impacts the gut:
Baseline gut integrity: A resilient gut barrier can tolerate occasional stressors. When the lining is already compromised, gluten is more likely to worsen permeability and inflammation.
Gut microbiome balance: The composition of gut bacteria plays a major role in how gluten proteins are processed. Dysbiosis can amplify inflammatory responses and weaken barrier function.
Genetic susceptibility: Certain genetic patterns increase immune reactivity to gluten, even in the absence of celiac disease. These individuals may experience symptoms without classic lab markers.
Immune system tone: Chronic inflammation, infections, or autoimmune tendencies can prime the immune system to overreact to otherwise tolerated foods.
Lifestyle and environmental stressors: Chronic stress, poor sleep, nutrient deficiencies, medications, and chemical exposures such as glyphosate can all lower the gut’s tolerance threshold.
Because these factors often overlap, gluten sensitivity can evolve over time. A person who once tolerated gluten may develop symptoms after prolonged stress, illness, hormonal changes, or repeated antibiotic use. This is why symptoms can feel inconsistent or unpredictable.
Understanding these individual differences is essential. It shifts the focus away from blaming a single food and toward restoring the conditions that allow the gut barrier and immune system to function properly. When those foundations are supported, reactions often become less severe—and in some cases, more manageable over time.
→ Advanced Functional Lab Testing
→ Functional & Integrative Medicine
5 Signs Your Leaky Gut May Be Triggered by Gluten
Gluten-related leaky gut does not look the same in everyone. Symptoms can be digestive, systemic, or both—and they often worsen gradually. The following signs commonly point to gluten as a contributing trigger.
Digestive symptoms flare after eating gluten
Bloating, gas, abdominal discomfort, diarrhea, or constipation that consistently worsen after consuming bread, pasta, or other gluten-containing foods are common early signals. These reactions may be delayed, making the connection easy to miss.
Skin issues that seem diet-related
Eczema, psoriasis, rashes, or unexplained itching can reflect underlying gut inflammation. When the gut barrier is compromised, immune activation can show up through the skin.
Brain fog and persistent fatigue
Difficulty concentrating, mental fog, or ongoing fatigue may stem from inflammatory signaling triggered by increased intestinal permeability. Many people are surprised to learn these symptoms can be gut-related.
Autoimmune symptoms that worsen with gluten
If you have an autoimmune condition and notice symptom flares after eating gluten, leaky gut may be amplifying immune reactivity. Increased permeability allows immune triggers greater access to circulation.
Joint pain or muscle aches without a clear cause
Inflammation originating in the gut can manifest as stiffness, joint discomfort, or muscle soreness, even in the absence of injury or overuse.
If several of these signs resonate, gluten may be contributing to ongoing gut barrier disruption rather than acting as a simple food sensitivity. Identifying this pattern is an important step toward meaningful healing.
→ Gut Health & Digestive Restoration
→ Functional & Integrative Medicine
What to Do If Gluten Is Wrecking Your Gut
If gluten is contributing to leaky gut, the goal is not just symptom relief—it’s restoring gut barrier integrity and calming immune activation. The steps below focus on removing ongoing triggers while actively supporting repair.
Go gluten-free the right way
Eliminating gluten is essential, but quality matters. Many gluten-free packaged foods are highly processed and can perpetuate inflammation. Prioritize naturally gluten-free, whole foods with short ingredient lists to reduce immune burden and support healing.
Focus on a gut-healing diet
Choose foods that provide the building blocks for repair and help rebalance the microbiome. Emphasize:
Bone broth and collagen-rich foods
Fermented foods to support microbial diversity
Wild-caught fatty fish for anti-inflammatory omega-3s
Organic fruits and vegetables
Seeds and fiber sources that nourish beneficial bacteria
Reduce refined sugars, seed oils, and ultra-processed foods that stress the gut lining.
Consider intermittent fasting
Strategic fasting gives the digestive system time to rest and repair. When done appropriately, it can reduce inflammatory signaling and support gut resilience. The approach should be individualized to avoid over-stressing the system.
Prioritize stress regulation
Stress directly weakens the gut barrier. Practices that activate the parasympathetic nervous system—such as gentle movement, breathwork, meditation, time in nature, and acupuncture—can meaningfully improve digestion and reduce permeability over time.
Address compounding factors
Medications, nutrient deficiencies, alcohol, and environmental exposures can all slow healing. Identifying and addressing these contributors helps prevent ongoing barrier disruption and supports more durable recovery.
Healing leaky gut is a process. Consistency with these foundational steps—paired with individualized support when needed—creates the conditions for the gut lining to repair and for symptoms to steadily improve.
→ Gut Health & Digestive Restoration
→ Acupuncture & Nervous System Regulation
→ Functional & Integrative Medicine
Personalized Gut Health Support
If you are dealing with ongoing digestive symptoms, fatigue, inflammation, or autoimmune flares—and suspect gluten may be playing a role—you do not have to navigate this alone.
A personalized, root-cause approach can help clarify:
Whether gluten is a primary trigger or one of several contributors
The extent of gut barrier disruption
What your gut needs to heal effectively and sustainably
Ready to Heal Your Gut at the Root Cause?
If you’re dealing with bloating, fatigue, food sensitivities, autoimmune flares, or lingering digestive symptoms—and suspect gluten may be contributing to leaky gut—you don’t have to figure this out on your own.
At Denver Sports & Holistic Medicine, we take a root-cause approach to gut health. That means looking beyond symptoms to identify what’s driving intestinal permeability, inflammation, and immune dysregulation, then creating a personalized plan to support true healing.
Care may include targeted functional testing, individualized nutrition strategies, gut-repair protocols, nervous system regulation, and acupuncture to support digestive and immune balance.
→ Gut Health & Digestive Restoration
→ Advanced Functional Lab Testing
→ Functional & Integrative Medicine
Request a free 15-minute consultation to discuss your symptoms, goals, and whether a personalized gut-healing approach is right for you.
Frequently Asked Questions About Gluten and Leaky Gut
What is leaky gut?
Leaky gut refers to increased intestinal permeability, a condition in which the gut lining becomes compromised and allows particles such as toxins, bacteria, and undigested food to pass into the bloodstream, triggering inflammation.
Can gluten cause leaky gut?
Yes. Gluten has been shown to increase the release of zonulin, a protein that loosens tight junctions in the intestinal lining. In susceptible individuals, this can contribute to increased gut permeability and inflammation.
Is leaky gut a real medical condition?
While leaky gut is not a formal diagnosis in conventional medicine, intestinal permeability is well documented in scientific research and is associated with autoimmune conditions, chronic inflammation, and digestive disorders.
How do I know if gluten is affecting my gut?
Common signs include bloating, gas, diarrhea or constipation after eating gluten, fatigue, brain fog, joint pain, skin issues, or worsening autoimmune symptoms. A structured elimination and clinical evaluation can help clarify gluten’s role.
Can you have leaky gut without digestive symptoms?
Yes. Some people experience non-digestive symptoms such as fatigue, headaches, joint pain, or autoimmune flares even when gastrointestinal symptoms are mild or inconsistent.
Does going gluten-free heal leaky gut?
Removing gluten can reduce ongoing irritation, but it does not automatically repair the gut lining. Healing often requires additional support for gut integrity, immune balance, nutrient status, and stress regulation.
How long does it take to heal a leaky gut?
Healing timelines vary. Some people notice improvement within a few months, while others may need longer depending on underlying causes, consistency, and overall lifestyle factors.
Can stress make leaky gut worse?
Yes. Chronic stress disrupts the gut microbiome, weakens the intestinal barrier, and increases inflammation, making the gut more vulnerable to food triggers such as gluten
Are gluten-free processed foods helpful for gut healing?
Not necessarily. Many gluten-free products are highly processed and can contain ingredients that irritate the gut. Whole, nutrient-dense foods are generally more supportive of gut repair
What is the goal of a holistic approach to gluten-related leaky gut?
The goal is to restore gut barrier integrity, reduce inflammation, support immune balance, and improve overall digestive resilience rather than relying on dietary restriction alone.
Resources
Leaky Gut and the Ingredients That Help Treat It: A Review - PMC
the Understanding of Gluten Sensitivity and Intolerance - PMC
The Role of Gluten in Gastrointestinal Disorders: A Review - PMC
The effect of wheat allergy on the course of atopic eczema in patients over 14 years of age - PubMed
Diet and Psoriasis: Part 2. Celiac Disease and Role of a Gluten-Free Diet - PMC