Is Gluten Making Your Gut Leaky? 5 Signs to Watch For and How to Heal Naturally
How Gluten Disrupts the Gut Lining, Increases Intestinal Permeability, and Drives Inflammation
If eating bread, pasta, or other gluten-containing foods leaves you bloated, fatigued, or mentally foggy, the issue may extend beyond simple food intolerance. In many individuals, gluten contributes to increased intestinal permeability—commonly referred to as leaky gut—by disrupting the gut’s protective barrier and activating immune and inflammatory pathways (1).
The intestinal lining is designed to be selectively permeable, allowing nutrients to pass through while preventing bacteria, toxins, and inflammatory compounds from entering circulation. This barrier is maintained by tight junctions that hold intestinal cells together and regulate what can cross into the bloodstream. When these junctions become compromised, immune-stimulating particles gain access to circulation, triggering inflammation that may manifest as digestive symptoms, fatigue, brain fog, skin issues, joint pain, or worsening autoimmune activity (2).
What makes gluten-related gut damage easy to overlook is that symptoms are often delayed, subtle, or non-digestive. Some people tolerate gluten for years before problems emerge, while others eliminate gluten yet continue to experience symptoms that fail to fully resolve. In these cases, persistent issues often reflect ongoing gut barrier dysfunction rather than gluten exposure alone (3).
While non-celiac gluten sensitivity is frequently discussed, this article focuses more specifically on how gluten directly affects the intestinal lining, increases permeability, and contributes to immune dysregulation and autoimmune disease risk (4). Rather than framing gluten as an isolated trigger, the goal is to understand how gut barrier damage develops, the systemic symptoms that can result, and what is required to support effective intestinal healing within a root-cause, systems-based framework.
→ Gut Health & Digestive Restoration
What Is Leaky Gut Syndrome? A Clinical Explanation
Intestinal Permeability and the Gut Barrier
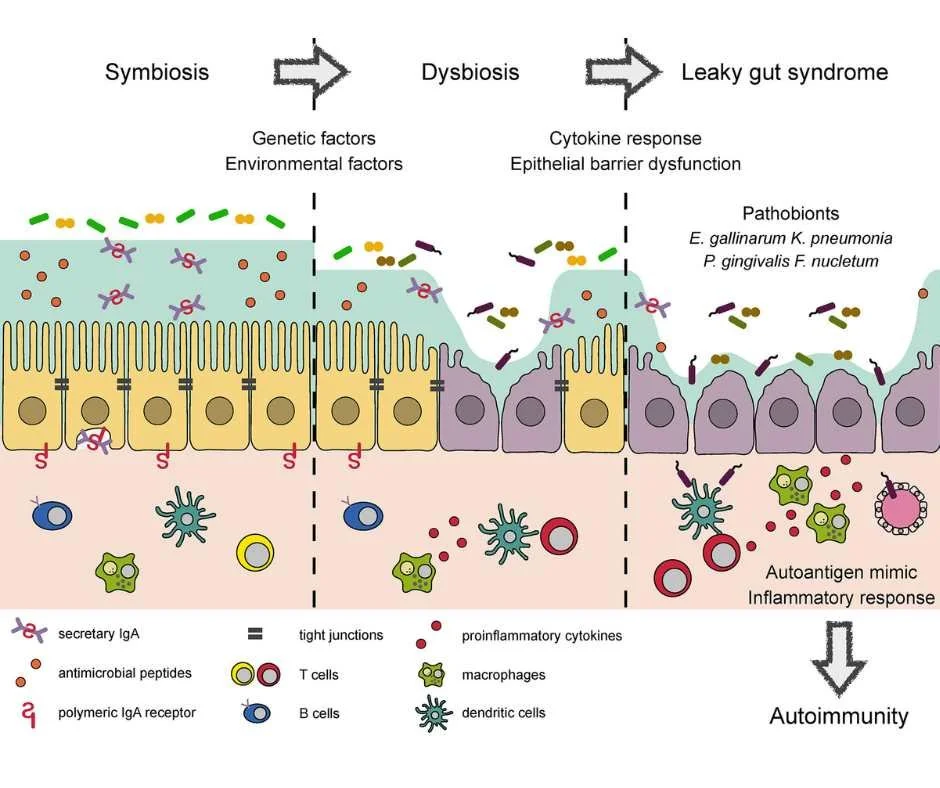
Leaky gut syndrome refers to increased intestinal permeability—a condition in which the protective lining of the small intestine becomes compromised. Under healthy conditions, this lining functions as a highly selective barrier, allowing nutrients, electrolytes, and water to enter the bloodstream while preventing bacteria, toxins, and partially digested food particles from escaping the gut lumen.
This selective permeability is essential for immune tolerance and metabolic balance. When intact, the gut barrier supports efficient nutrient absorption while limiting inappropriate immune activation (5).
The Role of Tight Junctions in Gut Integrity
Gut barrier integrity is maintained by several coordinated components, including the intestinal epithelial cells, the mucus layer, immune signaling within the gut-associated lymphoid tissue (GALT), and—most critically—the tight junctions that seal the spaces between adjacent intestinal cells.
Tight junctions are dynamic structures that respond to immune signals, microbial metabolites, nutrients, and stress hormones. When properly regulated, they allow the gut to adapt to physiological demands without compromising immune balance. Problems arise when tight junction signaling becomes dysregulated, allowing excessive permeability rather than controlled passage (6).
How Increased Intestinal Permeability Triggers Immune Activation
When intestinal permeability increases, substances that should remain confined to the gut—such as bacterial fragments, dietary antigens, and environmental toxins—can cross into circulation. The immune system identifies these particles as threats, triggering inflammatory and immune responses.
Over time, repeated immune activation places sustained pressure on regulatory systems, contributing not only to digestive symptoms but also to systemic manifestations involving the skin, joints, brain, endocrine system, and immune system as a whole (7). This helps explain why individuals may experience fatigue, cognitive symptoms, joint pain, or autoimmune flares even in the absence of prominent gastrointestinal complaints.
Why Leaky Gut Affects the Whole Body
Research has linked increased intestinal permeability to a wide range of chronic conditions, including inflammatory bowel disease, autoimmune disorders, metabolic dysfunction, cardiovascular disease, and neuroinflammatory processes. Importantly, leaky gut is not considered a disease itself, but rather a pathophysiological mechanism that amplifies inflammation and immune dysregulation across multiple systems (8).
Understanding leaky gut helps explain why symptoms are often widespread and why treating isolated complaints frequently falls short. Meaningful improvement requires restoring gut barrier integrity, calming immune activation, and addressing the underlying factors that disrupted the intestinal lining in the first place—rather than focusing solely on symptom suppression.
How Gluten Can Worsen Intestinal Permeability
Gluten, Zonulin, and Tight Junction Dysregulation
Gluten can be a significant driver of leaky gut because of how it interacts with proteins that regulate the intestinal barrier. One of the key regulators involved is zonulin, a signaling molecule that controls the opening and closing of tight junctions between intestinal cells (9).
In susceptible individuals, gluten exposure stimulates zonulin release, causing tight junctions to loosen beyond normal physiological control. Repeated activation of this pathway increases intestinal permeability, allowing inflammatory particles to cross the gut barrier and activate the immune system. Over time, this process can perpetuate chronic inflammation and interfere with proper repair of the intestinal lining.
Factors That Amplify Gluten-Related Gut Damage
Gluten rarely acts in isolation. Several physiological and environmental stressors can amplify its effects and further weaken gut barrier integrity, including:
Chronic stress, which alters gut motility, blood flow, and immune signaling
Glyphosate exposure from conventionally grown wheat and other crops, which can disrupt the gut microbiome and impair epithelial integrity (10)
Alcohol consumption, which increases intestinal permeability and inflammatory signaling
Medications such as NSAIDs, antibiotics, and hormonal birth control, all of which can compromise gut barrier function
Nutrient deficiencies—particularly vitamin D, zinc, and magnesium—which are essential for maintaining tight junction stability
When these stressors overlap, even modest gluten exposure may exceed the gut’s capacity to maintain a healthy intestinal barrier. This helps explain why some individuals tolerate gluten for years before symptoms emerge, and why reactions often worsen during periods of high stress, illness, or increased toxic burden.
Why Gluten Avoidance Alone Is Often Not Enough
Because multiple factors influence gut permeability, addressing gluten-related leaky gut requires more than dietary avoidance alone. Restoring gut resilience involves identifying and reducing ongoing stressors that continue to drive intestinal permeability and immune activation, while simultaneously supporting barrier repair and regulatory balance.
Why Gluten Affects Everyone Differently
Individual Differences in Gut and Immune Function
Gluten affects people differently because gut barrier integrity, immune regulation, genetics, and environmental exposures vary widely between individuals. Some people experience obvious digestive symptoms, while others develop fatigue, brain fog, joint pain, or autoimmune flares. Still others may appear to tolerate gluten for years before problems emerge. This variability is not random—it reflects differences in underlying biological terrain (11).
Factors That Shape Individual Gluten Tolerance
Several interconnected factors influence how gluten impacts the gut and immune system:
Baseline gut integrity
A resilient intestinal barrier can tolerate occasional stressors. When the gut lining is already compromised, gluten is more likely to worsen permeability and inflammation.Gut microbiome balance
The composition and diversity of gut bacteria influence how gluten proteins are processed. Dysbiosis can amplify inflammatory signaling and weaken barrier function.Genetic susceptibility
Certain genetic patterns increase immune reactivity to gluten even in the absence of celiac disease, leading to symptoms without classic diagnostic findings.Immune system tone
Chronic inflammation, persistent infections, or autoimmune tendencies can prime the immune system to overreact to otherwise tolerated foods.Lifestyle and environmental stressors
Factors such as chronic stress, poor sleep, medication use, nutrient depletion, and chemical exposures can progressively lower the gut’s tolerance threshold.
Why Gluten Sensitivity Can Change Over Time
Because these influences often overlap, gluten sensitivity frequently develops gradually rather than suddenly. Someone who once tolerated gluten may begin reacting after prolonged stress, illness, hormonal changes, or repeated antibiotic exposure. This helps explain why symptoms may feel inconsistent, delayed, or unpredictable (12).
Understanding this variability shifts the focus away from blaming a single food and toward restoring gut and immune resilience. When foundational systems are supported, reactions often become less severe—and, in some cases, more manageable over time.
5 Signs Your Leaky Gut May Be Triggered by Gluten
Gluten-related leaky gut can present with digestive, systemic, or immune-driven symptoms that often worsen gradually over time. Unlike IgE-mediated food allergies, which cause immediate reactions, gluten-related gut dysfunction typically involves delayed immune activation driven by increased intestinal permeability, rather than a classic allergic response (13).
The signs below suggest gluten may be acting as a contributing trigger, not merely an isolated food sensitivity.
Digestive symptoms that flare after eating gluten
Bloating, gas, abdominal discomfort, diarrhea, or constipation that reliably worsen after consuming bread, pasta, or other gluten-containing foods are common early indicators. Symptoms may be delayed by hours or even days, making the connection easy to overlook.
Skin issues that appear diet-related
Eczema, psoriasis, acne, rashes, or unexplained itching can reflect underlying gut-driven inflammation. When intestinal permeability increases, immune activation may manifest through the skin rather than the digestive tract.
Brain fog and persistent fatigue
Difficulty concentrating, mental fog, or ongoing fatigue may result from inflammatory signaling associated with increased intestinal permeability. These symptoms are frequently misattributed to stress, poor sleep, or aging rather than gut dysfunction.
Autoimmune symptoms that worsen with gluten
For individuals with autoimmune conditions, symptom flares following gluten exposure may indicate that leaky gut is amplifying immune reactivity. Increased permeability allows immune-stimulating particles greater access to circulation, intensifying inflammatory responses (14).
Joint pain or muscle aches without a clear cause
Inflammation originating in the gut can present as joint stiffness, pain, or muscle soreness, even in the absence of injury or overuse. This reflects the systemic reach of gut-driven immune activation.
If several of these patterns resonate, gluten may be contributing to ongoing gut barrier disruption rather than acting as a simple intolerance. In these cases, patterns over time matter more than isolated reactions—particularly when symptoms fluctuate, escalate, or involve multiple body systems.
How to Heal Leaky Gut When Gluten Is a Trigger
If gluten is contributing to leaky gut, the goal is not simply symptom relief—it is restoring gut barrier integrity and calming immune activation. Effective healing focuses on reducing ongoing stressors while actively supporting repair processes within the intestinal lining.
How to Go Gluten-Free Without Slowing Gut Healing
Eliminating gluten is an important first step, but food quality matters. Many packaged gluten-free products are highly processed and can perpetuate inflammation rather than support healing. Emphasizing naturally gluten-free, whole foods with simple ingredient lists helps reduce immune burden and creates a more supportive environment for gut repair (15).
Foods That Support Gut Barrier Repair
Choose foods that provide the structural and microbial support needed for intestinal recovery. Foundational components often include:
Bone broth and collagen-rich foods to support the gut lining
Fermented foods to encourage microbial balance
Wild-caught fatty fish for anti-inflammatory omega-3 fatty acids
Organic fruits, vegetables, and fiber-rich whole foods
At the same time, limiting refined sugars, industrial seed oils, and ultra-processed foods helps reduce additional inflammatory stress on the gut barrier (16).
Can Intermittent Fasting Help Heal Leaky Gut?
When used appropriately, intermittent fasting can give the digestive system time to rest, reduce inflammatory signaling, and support repair processes (17). This approach should be individualized, as excessive or poorly timed fasting may increase physiological stress and slow healing in some individuals.
How Stress Affects Gut Permeability—and Why Regulation Matters
Stress has a direct and measurable impact on gut barrier function through neuroimmune signaling pathways (18). Practices that support parasympathetic nervous system activation—such as gentle movement, breathwork, meditation, time in nature, and acupuncture—can improve digestion, support immune balance, and reduce intestinal permeability over time.
Other Factors That Prevent Leaky Gut Healing
Medications, alcohol intake, nutrient depletion, and environmental exposures can all interfere with gut healing. Identifying and addressing these contributors helps prevent ongoing barrier disruption and supports more durable, long-term improvement (19).
Healing leaky gut is a process rather than a quick fix. Consistent application of these foundational strategies—combined with individualized guidance when appropriate—creates the conditions necessary for gut barrier repair and sustained symptom improvement.
→ Functional & Integrative Medicine
When Gluten-Related Gut Symptoms Don’t Fully Resolve
If you are experiencing persistent digestive symptoms, fatigue, inflammation, or autoimmune flares—and suspect gluten may be playing a role—this often signals that gut barrier dysfunction and immune activation have not been fully addressed.
A personalized, root-cause approach can help clarify what is truly driving ongoing symptoms, including:
Whether gluten is a primary trigger or one contributing factor among several
The degree of intestinal permeability and immune dysregulation involved
Which targeted supports are needed to promote effective and sustainable healing
At Denver Sports & Holistic Medicine, care is centered on identifying the underlying contributors to intestinal permeability, inflammation, and immune dysregulation rather than relying on symptom suppression alone. Treatment plans are individualized to address the specific physiological, environmental, and lifestyle factors influencing gut resilience and overall health.
If gluten-related gut symptoms have been persistent, inconsistent, or difficult to resolve, a brief conversation can help determine whether further evaluation or personalized support may be appropriate.
You may request a free 15-minute consultation with Dr. Martina Sturm to review your health concerns and outline appropriate next steps within a root-cause, systems-based framework.
Frequently Asked Questions About Gluten and Leaky Gut
What is leaky gut?
Leaky gut refers to increased intestinal permeability, a condition in which the gut lining becomes compromised and allows particles such as toxins, bacteria, and undigested food to pass into the bloodstream, triggering inflammation.
Can gluten cause leaky gut?
Yes. Gluten has been shown to increase the release of zonulin, a protein that loosens tight junctions in the intestinal lining. In susceptible individuals, this can contribute to increased gut permeability and inflammation.
Is leaky gut a real medical condition?
While leaky gut is not a formal diagnosis in conventional medicine, intestinal permeability is well documented in scientific research and is associated with autoimmune conditions, chronic inflammation, and digestive disorders.
How do I know if gluten is affecting my gut?
Common signs include bloating, gas, diarrhea or constipation after eating gluten, fatigue, brain fog, joint pain, skin issues, or worsening autoimmune symptoms. A structured elimination and clinical evaluation can help clarify gluten’s role.
Can you have leaky gut without digestive symptoms?
Yes. Some people experience non-digestive symptoms such as fatigue, headaches, joint pain, or autoimmune flares even when gastrointestinal symptoms are mild or inconsistent.
Does going gluten-free heal leaky gut?
Removing gluten can reduce ongoing irritation, but it does not automatically repair the gut lining. Healing often requires additional support for gut integrity, immune balance, nutrient status, and stress regulation.
How long does it take to heal a leaky gut?
Healing timelines vary. Some people notice improvement within a few months, while others may need longer depending on underlying causes, consistency, and overall lifestyle factors.
Can stress make leaky gut worse?
Yes. Chronic stress disrupts the gut microbiome, weakens the intestinal barrier, and increases inflammation, making the gut more vulnerable to food triggers such as gluten
Are gluten-free processed foods helpful for gut healing?
Not necessarily. Many gluten-free products are highly processed and can contain ingredients that irritate the gut. Whole, nutrient-dense foods are generally more supportive of gut repair
What is the goal of a holistic approach to gluten-related leaky gut?
The goal is to restore gut barrier integrity, reduce inflammation, support immune balance, and improve overall digestive resilience rather than relying on dietary restriction alone.
Still Have Questions?
If the topics above reflect ongoing symptoms or unanswered concerns, a brief conversation can help clarify whether a root-cause approach is appropriate.
Resources
Nutrients – Leaky gut syndrome and nutritional compounds that support intestinal barrier integrity
Trends in Food Science & Technology – Pathogenesis of celiac disease and other gluten-related disorders and mitigation strategies
BMC Medicine – Non-celiac gluten sensitivity: current concepts and clinical relevance
Nature Reviews Gastroenterology & Hepatology – Genetic susceptibility and immune mechanisms in gluten sensitivity and intolerance
Environmental Health Perspectives – Glyphosate exposure and effects on the human gut microbiota
Gastroenterology – The role of gluten in gastrointestinal disorders
Journal of the European Academy of Dermatology and Venereology – Wheat allergy and its influence on atopic eczema in adolescents and adults