The Mold Detox Diet: What to Eat and Avoid to Reduce Dietary Mycotoxins
How targeted food choices influence dietary mycotoxin load, inflammation, and detoxification during mold recovery
Mold illness is often discussed in terms of indoor air quality and water-damaged buildings, but food is another significant—and frequently overlooked—source of exposure. Certain foods can increase mycotoxin burden, fuel inflammation, and slow recovery, while others help support detoxification, immune balance, and gut repair.
For individuals experiencing mold-related symptoms, diet is not a cure on its own. Environmental exposure must be addressed first. However, nutrition plays a critical supportive role by reducing ongoing dietary mycotoxin exposure, stabilizing inflammatory responses, and supplying the nutrients required for detoxification and tissue repair.
A mold detox diet is not about extreme restriction or long-term deprivation. It is a strategic, temporary dietary framework designed to:
minimize dietary sources of mycotoxins
reduce inflammatory load
support detoxification pathways and immune resilience
This article focuses specifically on how food choices influence mold recovery—what to avoid, what to prioritize, and how to approach diet safely while healing. The emphasis here is on reducing dietary mycotoxin exposure, calming inflammation, and supporting detoxification pathways as part of a broader, well-sequenced recovery plan.
How Diet Influences Mycotoxin Load, Inflammation, and Recovery in Mold Illness
Addressing the source of mold exposure is essential, but nutrition plays a foundational role in supporting recovery. Dietary choices influence inflammation, gut barrier integrity, immune signaling, and the body’s capacity to process and eliminate toxins.
When used appropriately, a mold-focused dietary approach supports healing in three key ways: (3)
How Reducing Dietary Mycotoxins Lowers Total Toxic Load
Mold exposure can lead to the accumulation of mycotoxins in the body. A mold-supportive diet reduces ongoing dietary exposure by limiting foods more likely to harbor mold or fermentation-related toxins, such as aged cheeses, fermented products, and alcohol. Lowering this incoming burden allows detoxification pathways to focus on clearing existing toxins rather than continually managing new ones.
Why Mold Illness Depletes Nutrients and Increases Metabolic Demand
Mold illness is commonly associated with nutrient depletion due to chronic inflammation, gut dysfunction, and increased detoxification demands. Emphasizing nutrient-dense whole foods—including vegetables, healthy fats, quality proteins, and key micronutrients—helps support tissue repair, mitochondrial function, and immune resilience.
How Anti-Inflammatory Foods Support Immune Regulation During Mold Recovery
Chronic mold exposure can drive persistent inflammatory signaling that disrupts immune regulation. Anti-inflammatory dietary strategies, including fiber-rich vegetables and omega-3 fatty acids, help calm inflammation and support immune recovery without overstimulation.
Nutrition does not resolve mold illness on its own, but it provides a critical foundation that supports detoxification, improves tolerance to treatment, and enhances recovery when combined with appropriate environmental and clinical care.
Because mold illness often involves immune dysregulation, gut dysfunction, and impaired detoxification, dietary strategies are most effective when integrated into a comprehensive, individualized care plan.
→ Mold Illness & Environmental Toxicity
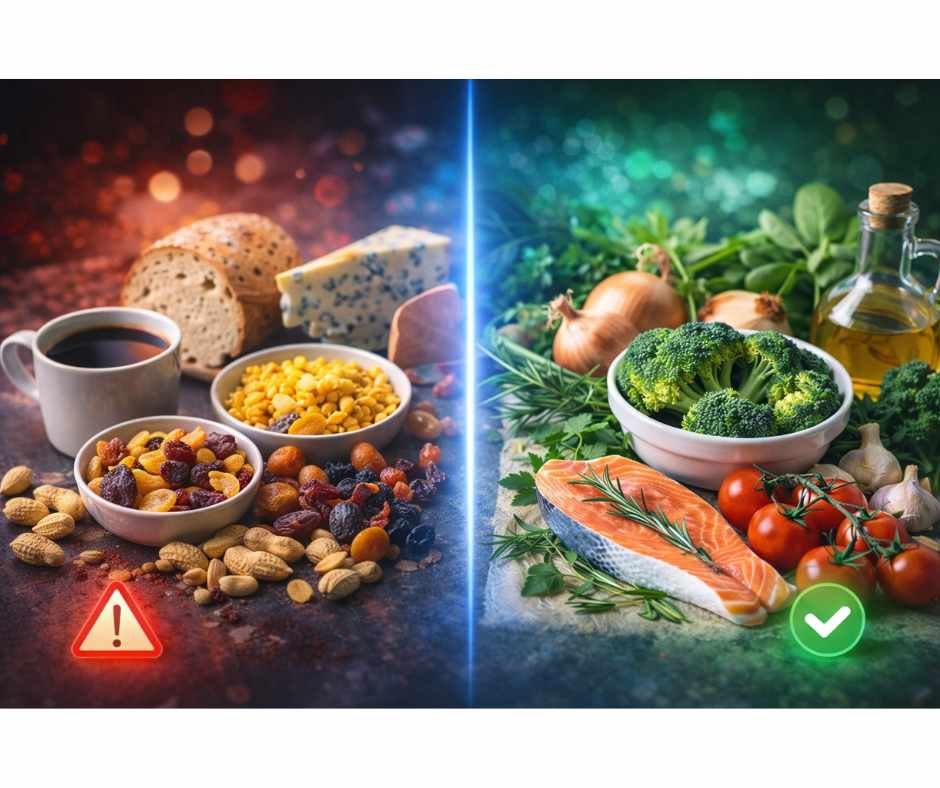
Foods That Increase Mycotoxin Exposure and Inflammatory Burden During Mold Detox
During mold recovery, food choices can either reduce physiological stress or perpetuate inflammatory and detoxification bottlenecks. The following categories are commonly problematic because they increase mycotoxin exposure, impair gut barrier integrity, disrupt immune signaling, or overwhelm detox pathways already under strain.
Why Ultra-Processed Foods Increase Inflammation and Detox Burden
Ultra-processed foods often contain hidden sugars, refined carbohydrates, industrial seed oils, and preservatives that worsen neuroinflammation, disrupt gut barrier integrity, and impair detoxification pathways. (4) These foods also increase oxidative stress and mitochondrial strain, compounding the inflammatory burden created by mold exposure and slowing recovery.
How Sugar and Refined Carbohydrates Fuel Fungal and Microbial Overgrowth
Sugar serves as a readily available fuel source for mold, yeast, and dysbiotic microbes. Excess intake can worsen symptoms, destabilize blood sugar, and intensify cravings—often reflecting ongoing fungal or mold-related imbalance.
Avoid the following sweeteners and high-glycemic foods:
Glucose
High-fructose corn syrup (HFCS)
Lactose
Fructose
Mannitol, sorbitol
Honey, maple syrup, molasses
Candy, baked goods, sweets
White breads and refined carbohydrates
High-sugar fruits should also be limited during active mold detox, as they can increase microbial fermentation and inflammatory signaling:
Bananas
Melons
Oranges
Grapes
Pineapple
Mango
Dried fruit and fruit juice
Why Gluten Can Worsen Gut Permeability and Immune Activation in Mold Illness
While not everyone with mold illness has celiac disease or non-celiac gluten sensitivity, gluten can significantly increase inflammatory burden and impair gut barrier function—both of which are already compromised in many individuals with mold-related illness.
For most individuals recovering from mold exposure, eliminating gluten-containing grains such as wheat, rye, and barley is advisable. (5) In susceptible individuals, gluten cross-reactive foods may further contribute to immune activation and delayed gut healing.
When symptoms persist or dietary responses are unclear, advanced functional testing can help clarify food sensitivities and overall toxic burden.
→ Advanced Functional Lab Testing
How Industrial Seed Oils Amplify Oxidative Stress and Immune Dysregulation
Seed oils such as soy, canola, sunflower, and corn oil are high in omega-6 fatty acids, which can promote inflammatory signaling, lipid peroxidation, and oxidative stress—factors that worsen immune dysregulation and detox strain in mold illness. (6)
Replace seed oils with healthier fat sources such as:
Olive oil
Avocado oil
Coconut oil
Ghee
Omega-3–rich foods
Foods Most Likely to Contain Dietary Mycotoxins
Certain foods are more prone to mold growth, improper storage contamination, or mycotoxin accumulation and are best avoided during active detoxification: (7)
Meat and dairy from grain-fed animals
Conventional coffee
Beer and wine
Peanuts and peanut butter
Corn and corn-based products
Dried fruit
Healthier alternatives may include:
Select nuts and seeds (used cautiously)
Organic spices
Organic loose-leaf herbal teas
High-quality, mold-tested coffee (introduced later, if tolerated)
Foods That Can Worsen Symptoms During Active Detox Phases
During periods of heightened sensitivity or active detoxification, additional foods may aggravate symptoms due to fermentation potential, histamine activity, or immune stimulation:
Vinegar and vinegar-based condiments
Soy sauce and fermented condiments
Aged or mold-ripened cheeses
Soy and wheat products
Potatoes
Mushrooms and yeast-containing foods
For individuals with persistent or severe symptoms, a short-term advanced elimination phase may also include:
All grains
Starchy vegetables
Fermented foods
Shelled nuts
Condiments containing sugar or vinegar
Sour milk products (e.g., sour cream)
Beverages That Increase Fermentation, Histamine, or Detox Load
Liquid sources of sugar, alcohol, or fermentation byproducts can significantly increase inflammatory and detox burden:
Sweetened beverages
Fruit juice
Alcohol
Fermented drinks (kombucha, cider)
Oolong and black tea
Foods That May Worsen Symptoms Depending on Gut Function and Detox Capacity
Some foods fall into a gray zone during mold recovery. They are not inherently problematic, but they may worsen symptoms depending on individual tolerance, gut function, microbial balance, and overall detox capacity. These foods are often best approached strategically rather than avoided indefinitely.
When Gluten-Free Grains Still Create Problems During Mold Recovery
Gluten-free grains such as brown rice, quinoa, and buckwheat may be tolerated by some individuals once acute inflammation has calmed. However, these foods can still pose challenges during mold recovery due to potential mold contamination during storage, carbohydrate load, and their impact on blood sugar regulation.
In sensitive individuals, even gluten-free grains may contribute to digestive symptoms, immune activation, or delayed detoxification. Careful sourcing, thorough rinsing, and gradual reintroduction are essential when including these foods.
Examples include:
Brown rice
Quinoa
Buckwheat
Why Legumes Can Increase Fermentation and Histamine Symptoms
Legumes such as beans, lentils, and chickpeas provide fiber and plant-based protein, but they can be difficult to tolerate during active mold detox. Their fermentable carbohydrate content may increase bloating, gas, or histamine-related symptoms in individuals with gut dysbiosis or impaired microbial balance.
If included, legumes are generally better tolerated after soaking, pressure cooking, and introduced in small amounts once digestive function and symptom stability improve.
Examples include:
Beans
Lentils
Chickpeas
How Even Low-Sugar Fruit Can Affect Symptoms in Sensitive Individuals
Lower-sugar fruits are often better tolerated than high-sugar options during mold recovery, but they can still provoke symptoms in some individuals due to fructose content or effects on microbial activity.
Berries, apples, and pears may be reintroduced cautiously once cravings, inflammation, and energy fluctuations have stabilized. Portion size and timing matter, and fruit is often better tolerated when paired with protein or healthy fats.
Examples include:
Berries
Apples
Pears
How to Reintroduce Foods Without Triggering Detox Setbacks
Tolerance varies widely, and these foods are best reintroduced gradually once inflammation and symptoms have stabilized. Introducing one food at a time, in small portions, allows for clearer symptom tracking and reduces the risk of triggering setbacks.
If symptoms flare consistently with reintroduction, it may signal unresolved gut dysfunction, microbial imbalance, or insufficient detox capacity—areas that often require individualized support rather than continued dietary restriction.
Foods That Support Detoxification, Immune Balance, and Gut Repair During Mold Recovery
A mold detox diet is not just about avoiding problematic foods—it is about strategic nourishment. The goal is to lower inflammatory load, support detoxification and elimination pathways, and provide the macronutrients and micronutrients required for immune regulation, gut repair, and cellular resilience during recovery.
Because mold illness often affects digestion, bile flow, and metabolic tolerance, foods that are clean, minimally processed, and nutrient-dense are typically best tolerated. The categories below form the foundation of a mold-supportive diet and can usually be eaten regularly unless individual sensitivities are present.
Why Non-Starchy Vegetables Support Detoxification and Gut Integrity
Vegetables
Non-starchy vegetables provide fiber, antioxidants, and phytonutrients that support liver detoxification, immune signaling, and gut barrier integrity—without significantly increasing microbial fermentation or blood sugar stress.
Leafy greens
Broccoli
Kale
Spinach
Arugula
Colorful vegetables
Bell peppers
Carrots
Beets
These vegetables support phase II detoxification pathways, provide minerals required for enzymatic activity, and help maintain regular bowel elimination—an essential component of mycotoxin clearance.
Protein Sources That Support Glutathione Production and Tissue Repair
Adequate protein intake is critical during mold recovery. Amino acids are required for detoxification enzymes, glutathione production, immune signaling, tissue repair, and neurotransmitter balance.
Preferred options
Wild-caught fish: salmon, sardines, herring, anchovies
Pasture-raised meats and eggs: organic, grass-fed/finished, and pasture-raised when possible
Consistent, well-tolerated protein intake helps stabilize blood sugar, reduce inflammatory stress, and support resilience during detoxification.
Healthy Fats That Support Bile Flow and Mycotoxin Elimination
Healthy fats play a central role in mold recovery by supporting bile production, hormone signaling, nervous system stability, and toxin elimination through the gastrointestinal tract.
Well-tolerated fat sources
Butter (preferably grass-fed)
Avocado and avocado oil
Olives and olive oil
Ghee
Coconut oil
Tallow
Including sufficient dietary fat supports the transport and elimination of fat-soluble mycotoxins and helps reduce detox-related symptom flares associated with poor bile flow.
Herbs and Spices That Support Immune Balance Without Fermentation Risk
Culinary herbs and spices can provide gentle antimicrobial, anti-inflammatory, and antioxidant support without the risks associated with fermented or mold-prone foods, when sourced carefully.
Commonly well tolerated
Turmeric
Parsley
Cloves
Cumin
Rosemary
Sage
Thyme
Oregano
Basil
Bay leaf
These compounds support immune balance and oxidative stress regulation while enhancing flavor, making dietary changes more sustainable.
How Bitter Foods Can Improve Digestion and Detox Tolerance
Bitter compounds stimulate digestive secretions and bile flow, supporting detoxification and nutrient absorption. Tolerance varies, particularly in individuals with histamine sensitivity or nervous system dysregulation.
Examples
Green tea
Mold-tested coffee
Bitter dark chocolate (used cautiously due to potential heavy metal content)
When tolerated, bitters can enhance digestive efficiency and support elimination, but they are best introduced gradually and adjusted based on symptom response.
Adjunctive Strategies That May Support Mycotoxin Elimination Beyond Diet
Diet provides the foundation for mold recovery, but some individuals benefit from additional supportive strategies once ongoing exposure has been reduced and basic detox and elimination pathways are functioning adequately. These approaches are not universally required and are most effective when layered in thoughtfully rather than introduced all at once.
When and Why Binders Are Used to Support Mycotoxin Elimination
Binders such as activated charcoal, bentonite clay, modified citrus pectin, or chlorella may help bind mycotoxins within the gastrointestinal tract and support elimination through stool. Because different mycotoxins have varying chemical properties, no single binder is universally effective, and response can vary significantly between individuals.
Timing is critical. Introducing binders too early—or without adequate bile flow, hydration, and bowel regularity—can worsen symptoms by redistributing toxins rather than eliminating them. This risk is higher in individuals with constipation, impaired liver or gallbladder function, or heightened nervous system sensitivity.
For these reasons, binders are best introduced with practitioner guidance and adjusted based on symptom response.
Supplements That May Support Detox, Inflammation, and Histamine Balance
Certain supplements may support detoxification, inflammation regulation, and histamine balance when used appropriately and in the correct sequence. These may include:
Glutathione
Phosphatidylcholine
NAC (N-acetylcysteine)
Milk thistle extract
Quercetin
Diamine oxidase (DAO)
Spore-based probiotics
Digestive bitters
Supplement needs vary widely depending on mycotoxin burden, gut integrity, immune activation, and overall detox capacity. Introducing supplements without a clear clinical rationale or sequence can increase symptom volatility rather than support recovery, which is why individualized assessment matters.
Adjunctive Therapies That May Improve Detox Tolerance and Recovery
In some cases, additional therapies may be used to support nervous system regulation, circulation, and detoxification capacity as recovery progresses.
Acupuncture may support autonomic balance, digestive function, and liver-related energetic pathways, helping improve tolerance to detoxification.
Sauna therapy can promote circulation and sweating, offering an additional elimination route through the skin when hydration and mineral balance are adequate.
Ozone therapy, when medically administered and properly sequenced, may support immune modulation and mycotoxin neutralization in selected cases.
These therapies are not first-line interventions and require careful timing and professional oversight to avoid detox overload or symptom flares.
Why Mold Recovery Often Requires Personalized, Clinically Guided Support
Mold-related illness can feel overwhelming, particularly when symptoms affect multiple systems and continue despite well-intended dietary and lifestyle changes. While nutrition plays an important role in reducing exposure and calming inflammation, lasting improvement typically requires individualized guidance and careful clinical sequencing.
Mold illness is rarely isolated. It is often layered with immune dysregulation, gut imbalance, nervous system stress, and impaired detoxification capacity. Addressing these factors safely requires understanding how they interact—and when to introduce each level of support—starting with exposure identification and foundational stabilization before progressing to more advanced interventions.
You may request a free 15-minute consultation with Dr. Martina Sturm to review your health concerns and outline appropriate next steps within a root-cause, systems-based framework.
With the right approach and guidance, recovery is possible.
Frequently Asked Questions About the Mold Detox Diet
What is a mold detox diet?
A mold detox diet is a short-term, strategic nutrition plan designed to reduce dietary sources of mycotoxins, lower inflammation, support gut integrity, and provide nutrients that assist the body’s detoxification pathways during mold recovery.
How long should I follow a mold detox diet?
Timelines vary based on symptom severity, exposure level, and individual tolerance. Many people benefit from an initial structured phase followed by a gradual reintroduction process once symptoms stabilize and exposure sources are addressed.
Does a mold detox diet replace environmental remediation?
No. Diet can reduce dietary exposure and inflammatory load, but it cannot compensate for ongoing exposure in a water-damaged environment. Removing or remediating the exposure source remains foundational.
What foods are most commonly avoided on a mold detox diet?
Commonly avoided foods include ultra-processed foods, added sugars, gluten-containing grains, industrial seed oils, alcohol, and foods more prone to mold or fermentation-related issues such as aged cheeses, vinegar-based condiments, peanuts, corn, and some dried fruits.
Can I eat gluten-free grains during mold detox?
Some people tolerate gluten-free grains, while others do not. Certain grains can be more prone to mold contamination or may worsen symptoms due to carbohydrate load. Individual response and careful sourcing matter.
Do I need to avoid coffee during mold detox?
Some people benefit from avoiding conventional coffee due to mold contamination risk or symptom sensitivity. Others tolerate mold-tested coffee well. The decision depends on symptom response and product quality.
Why do symptoms sometimes worsen when I change my diet?
Symptom shifts can occur when inflammatory triggers are removed, gut function changes, or detoxification demand increases. This is one reason gradual changes and professional guidance can be helpful, especially for those with significant symptoms.
Are binders necessary during a mold detox diet?
Not always. Diet can be a strong first step. Binders may be introduced in some cases to support mycotoxin elimination, but timing and individual tolerance matter, and they are best used under practitioner guidance.
What is the best first step if I suspect mold-related illness?
The best first step is identifying potential exposure sources and reducing ongoing exposure where possible. From there, a structured nutrition plan and individualized evaluation can help clarify next steps.
Resources
Journal of Occupational and Environmental Medicine – Respiratory conditions associated with mold exposure and damp indoor environments
Institute for Functional Medicine – Mold toxicity: pathways, diseases, and clinical interventions
Nutrients – Dietary strategies and nutritional considerations in mold-related illness
Frontiers in Neuroscience – Overnutrition modulates lipopolysaccharide regulation of mycotoxin-induced neurotoxicity in neurodegenerative disease models
Gastroenterology – Celiac disease, wheat allergy, and non-celiac gluten sensitivity: clinical distinctions and implications
Diabetes – Soybean oil is more obesogenic and diabetogenic than coconut oil and fructose in murine models
Food and Chemical Toxicology – Occurrence, toxicity, and analytical assessment of major mycotoxins in food