Endometriosis: A Functional Medicine Perspective on Root Causes and Whole-System Support
How immune dysfunction, progesterone resistance, inflammation, and environmental exposures contribute to endometriosis—and why symptom-only treatment often falls short
Whether you have been suffering quietly for years or are among the estimated 10–15% of reproductive-aged women diagnosed with endometriosis, this condition can significantly affect daily life, long-term health, and overall well-being (1).
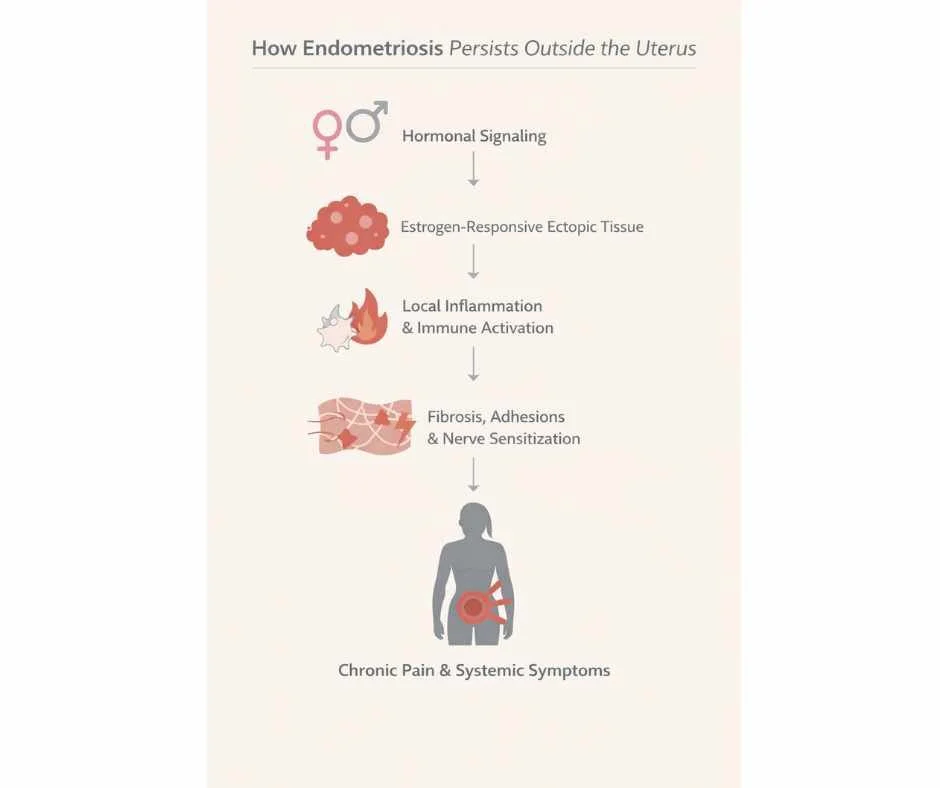
Chronic pelvic pain, painful periods, fatigue, digestive discomfort, and fertility challenges are not isolated symptoms. In endometriosis, they reflect deeper inflammatory, immune, and hormonal signaling disturbances that often extend beyond the reproductive system.
From a functional medicine perspective, endometriosis reflects a hormonally responsive, immune-mediated inflammatory state that develops and persists when regulatory systems remain disrupted—and can improve or resolve when those underlying drivers are adequately addressed.
This article discusses how endometriosis develops as a hormonally responsive, immune-mediated inflammatory condition, why symptoms often persist despite conventional treatment, and how a functional medicine framework evaluates contributing factors without relying on symptom suppression alone.
What Is Endometriosis?
Endometriosis is a chronic inflammatory condition in which tissue resembling the endometrium—the lining of the uterus—implants and grows outside the uterine cavity. These endometrial-like implants are most commonly found on the ovaries, fallopian tubes, pelvic peritoneum, rectovaginal space, and, in some cases, the bowel or bladder (2).
Importantly, endometriosis is not simply misplaced uterine tissue. Research has shown that these ectopic lesions differ biologically from normal endometrial cells, exhibiting altered immune signaling, abnormal inflammatory activity, and distinct hormone receptor behavior. This helps explain why endometriosis can persist, progress, and cause significant symptoms even when circulating hormone levels appear normal.
Endometriosis is now recognized as a condition involving aberrant tissue behavior within a dysregulated biological environment, rather than a purely anatomical problem.
How Endometrial-Like Tissue Behaves Outside the Uterus
Endometriotic lesions remain hormonally responsive, particularly to estrogen. During the menstrual cycle, these tissues thicken and react to cyclical hormonal signaling in a manner similar to uterine endometrium. However, unlike uterine tissue, ectopic lesions have no physiologic pathway for breakdown or clearance.
As a result, repeated cycles of stimulation lead to:
Persistent local inflammation
Swelling and oxidative stress
Fibrotic tissue remodeling
Adhesion formation between organs
Over time, this inflammatory cascade contributes to chronic pelvic pain, restricted organ mobility, and progressive symptom burden (3). In addition, inflammatory mediators released by these lesions can sensitize surrounding nerves, amplifying pain perception even when lesion size is relatively small.
This helps explain why symptom severity does not always correlate with the visible extent of disease.
Why Endometriosis Is More Than a Gynecologic Condition
Although endometriosis is often categorized as a reproductive disorder, current research supports its classification as a systemic, immune-mediated inflammatory condition.
Endometriosis involves:
Altered immune surveillance that fails to clear ectopic tissue
Chronic inflammatory signaling within the pelvic environment
Abnormal hormone receptor responsiveness at the tissue level
Nervous system sensitization that can perpetuate pain beyond the pelvis
These overlapping mechanisms mean that endometriosis affects far more than reproductive anatomy alone. Fatigue, pain amplification, bowel or bladder symptoms, and widespread inflammatory effects reflect the involvement of multiple regulatory systems—not just the uterus or ovaries.
Understanding endometriosis through this broader biological lens is essential for explaining why symptom-only approaches often fall short and why whole-system evaluation is necessary for meaningful, sustained improvement.
Who Is Most Affected by Endometriosis
Endometriosis affects approximately 1 in 10 menstruating women in the United States, making it one of the most common gynecologic conditions worldwide (4). Although diagnosis most often occurs in women in their 30s and 40s, symptom onset frequently begins much earlier—sometimes in adolescence.
A hallmark challenge in endometriosis care is diagnostic delay, with many women waiting an average of 7 to 10 years between initial symptom onset and formal diagnosis. During this time, disease activity and inflammatory burden may continue to progress.
Prevalence, Age Patterns, and Diagnostic Delays
Delayed diagnosis is common because early symptoms—such as painful periods, pelvic discomfort, fatigue, or gastrointestinal changes—are often normalized or attributed to routine menstrual variation. In other cases, symptoms may be treated in isolation without investigation into an underlying inflammatory condition.
These delays matter. Prolonged untreated inflammation can contribute to lesion persistence, adhesion formation, and nervous system sensitization, helping explain why symptoms may intensify or broaden over time before appropriate care is initiated.
Genetic and Familial Risk Factors
Endometriosis demonstrates a clear familial pattern. Women with a first-degree relative (mother, sister, or daughter) diagnosed with endometriosis have a significantly higher risk of developing the condition themselves (9).
Importantly, genetic susceptibility does not act as a sole cause. Instead, inherited factors appear to influence immune regulation, inflammatory signaling, and hormone receptor responsiveness, shaping how the body responds to endometrial-like tissue outside the uterus. This helps explain why endometriosis can present differently—even among women within the same family.
Common Signs and Symptoms of Endometriosis
Endometriosis presents with a wide range of symptoms, and symptom severity does not reliably correlate with the extent of visible disease. Some individuals with extensive lesions report mild discomfort, while others experience debilitating pain with minimal findings on imaging or surgery.
This variability reflects differences in inflammatory activity, immune response, lesion location, and nervous system sensitization rather than disease burden alone.
Pelvic and Menstrual Symptoms
Pelvic and menstrual symptoms are the most commonly recognized features of endometriosis and often prompt initial evaluation.
These may include:
Painful menstrual cramping that worsens over time
Heavy or prolonged menstrual bleeding
Persistent pelvic pain between cycles
Pain during or after intercourse
Pain with bowel movements or urination during menstruation (5)
Pain patterns may fluctuate across the menstrual cycle and can intensify as inflammatory signaling and tissue irritation accumulate.
Non-Pelvic and Systemic Symptoms
Because endometriosis involves inflammatory and immune-mediated processes, symptoms are not always confined to the pelvis.
Non-pelvic symptoms may include:
Chronic fatigue
Low back or hip pain
Abdominal bloating or constipation
Spotting or irregular bleeding between cycles
These symptoms can reflect referred pain, inflammatory spillover, or nervous system involvement, rather than primary disease in those tissues.
Some individuals experience relatively mild or intermittent symptoms, while others develop progressively worsening pain, fatigue, and functional limitation over time. Recognizing the full symptom spectrum is essential for understanding why endometriosis is often underdiagnosed and inadequately managed when evaluation focuses narrowly on reproductive anatomy alone.
Why Endometriosis Often Progresses Over Time
Endometriosis is widely understood as a chronic inflammatory condition rather than a static gynecologic finding. When the biological drivers that support lesion survival remain unaddressed, inflammatory activity can persist from cycle to cycle, allowing disease processes to continue even when symptoms fluctuate.
Over time, repeated inflammatory signaling can alter local tissue structure, pain perception, and organ function—contributing to progression that may not be immediately visible on imaging or during routine evaluation.
Chronic Inflammation and Adhesion Formation
Persistent inflammation within the pelvic environment promotes fibrosis and adhesion formation, in which connective tissue develops between organs and surrounding structures. These adhesions can restrict normal organ mobility, alter biomechanics within the pelvis, and create ongoing mechanical tension that amplifies pain patterns (3).
As fibrosis accumulates, tissues may become less responsive to short-term symptom relief strategies, increasing the likelihood of chronic or recurrent pain.
Why Symptoms Can Worsen Even With Symptom Suppression
Symptom-focused approaches—such as pain medications or hormonal suppression—may reduce discomfort temporarily but often do not address the immune dysregulation, inflammatory signaling, or lesion persistence that sustain endometriosis activity.
As a result, inflammatory processes may continue beneath the surface, allowing tissue irritation, nerve sensitization, and fibrosis to progress even when pain appears controlled. This helps explain why symptoms may return, broaden, or intensify over time despite ongoing treatment.
Why this matters clinically
Understanding progression reframes endometriosis as a condition that requires upstream evaluation, not simply escalating symptom management. This perspective is central to explaining why many individuals experience ongoing challenges despite multiple interventions—and why a whole-system lens becomes increasingly important as symptoms evolve.
Possible Root Causes of Endometriosis
Current research suggests that endometriosis develops through the interaction of multiple biological systems, rather than from a single initiating cause. These interacting factors shape how endometrial-like tissue survives outside the uterus, how inflammation is sustained, and why symptoms persist or progress over time.
Rather than acting independently, hormonal signaling, immune regulation, genetics, and environmental exposures appear to reinforce one another within the endometriotic environment.
Progesterone Resistance and Estrogen Responsiveness
Endometriosis is increasingly understood to involve progesterone resistance, a state in which tissues do not respond appropriately to progesterone’s anti-inflammatory and regulatory effects. When this signaling is impaired, estrogen-responsive tissue activity is less effectively counterbalanced, allowing inflammatory processes and lesion persistence to continue (6).
Importantly, this altered responsiveness occurs at the tissue level, helping explain why circulating hormone levels may appear normal despite ongoing disease activity.
Immune Dysregulation and Inflammatory Signaling
Immune system dysfunction plays a central role in endometriosis. Studies examining peritoneal fluid in affected individuals demonstrate elevated inflammatory cytokines and reduced immune surveillance, limiting the body’s ability to recognize and clear ectopic endometrial-like tissue (8).
This impaired immune response allows lesions to survive in locations where they would normally be eliminated, perpetuating chronic inflammation within the pelvic environment.
Gut Microbiome Differences Observed in Endometriosis
Research has identified distinct gut microbiome patterns in women with endometriosis compared to those without the condition. These differences are thought to influence immune communication and estrogen metabolism, potentially contributing to sustained inflammatory signaling and lesion persistence (7).
While the direction of this relationship remains under investigation, these findings highlight the interconnected nature of immune and inflammatory regulation in endometriosis.
Genetic Susceptibility
Endometriosis demonstrates a clear familial pattern, supporting the presence of genetic susceptibility rather than deterministic inheritance. Identified genetic factors appear to influence inflammatory pathways, immune regulation, and hormone receptor behavior, shaping how the body responds to ectopic tissue rather than directly causing disease (9).
This helps explain why individuals with similar genetic backgrounds may experience different symptom severity or disease progression.
Environmental Endocrine Disruptors
Environmental exposures also contribute to endometriosis risk. Estrogen-mimicking chemicals known as endocrine disruptors, including phthalates, have been detected at higher levels in women with endometriosis (10).
These compounds may interfere with hormonal signaling and immune regulation, further supporting an inflammatory environment that favors lesion survival and disease persistence.
Why this framing matters
By viewing endometriosis through the lens of interacting biological drivers, this model explains why symptom-focused treatment alone often fails to produce lasting relief—and why evaluation must extend beyond reproductive anatomy to understand the full disease process.
A Functional Medicine Lens on Endometriosis
From a functional medicine perspective, endometriosis is best understood as a hormonally responsive, immune-mediated inflammatory condition that develops and persists within a complex biological environment. Rather than viewing lesions as isolated anatomical abnormalities, this approach examines the regulatory systems that allow endometrial-like tissue to survive, trigger inflammation, and generate pain over time.
This broader lens helps explain why symptom patterns vary widely between individuals and why disease activity may continue even when conventional treatments appear effective on the surface.
Why Symptom-Only Approaches Often Fall Short
Conventional management strategies—including NSAIDs, hormonal suppression, and surgical intervention—may reduce pain or lesion burden temporarily. However, these approaches often focus on downstream effects rather than the upstream drivers that sustain endometriosis activity.
When immune dysregulation, inflammatory signaling, or environmental influences remain unaddressed, lesion persistence and symptom recurrence become more likely. This helps explain why many individuals experience incomplete relief, recurrent pain, or progressive symptoms despite multiple interventions (11–14).
Evaluating Endometriosis as a Whole-System Condition
Functional evaluation considers how multiple regulatory systems interact in the context of endometriosis, including:
Hormonal signaling at the tissue level
Immune regulation and inflammatory activity
Detoxification capacity and environmental load
Nervous system sensitization and pain amplification
Rather than applying standardized protocols, this framework prioritizes identifying which contributors are most relevant for each individual and how they interact to influence symptom expression and disease progression.
Care at Denver Sports and Holistic Medicine is grounded in this systems-based approach, with evaluation focused on understanding the specific drivers influencing endometriosis activity and determining appropriate next steps.
→ Women’s Health & Fertility Support
Supportive Strategies Used in Functional Care
Functional approaches to endometriosis emphasize supporting regulatory systems rather than suppressing symptoms in isolation. The goal is not to override physiology, but to reduce biological stressors that perpetuate inflammation, tissue irritation, and pain signaling over time.
These strategies are used within a broader clinical framework and are individualized based on symptom patterns, tolerance, and overall health context. Importantly, they are not applied as standalone fixes, but as part of coordinated, systems-based care.
Pain Modulation and Inflammatory Load
Chronic inflammation plays a central role in endometriosis-related pain and symptom persistence. Certain botanical compounds—such as curcumin, ginger, and boswellia—have demonstrated anti-inflammatory effects comparable to nonsteroidal anti-inflammatory drugs in some studies, without the same degree of gastrointestinal risk (11,12,16).
Within functional care, these agents are considered for their ability to modulate inflammatory signaling and reduce pain amplification, rather than simply masking discomfort.
Antioxidant and Cellular Protection Support
Oxidative stress has been implicated in lesion persistence and inflammatory amplification in endometriosis. Nutrients including vitamins A, C, and E, along with compounds such as N-acetylcysteine and green tea polyphenols, support cellular resilience in inflammatory environments (13,15).
This type of support focuses on reducing cumulative tissue stress and protecting against ongoing inflammatory damage, rather than directly targeting lesions.
Liver Clearance and Hormone Metabolism Support
Hormonal signaling in endometriosis is influenced by how effectively estrogen is metabolized and cleared. These processes rely on adequate nutrient availability and bile flow. B vitamins and lipotropic compounds play supportive roles in these biochemical pathways and are often considered within a functional framework (17,18).
This support is context-dependent, integrated into broader assessment findings, and not applied uniformly across individuals.
Acupuncture and Traditional Chinese Medicine Perspectives
From a Traditional Chinese Medicine (TCM) perspective, endometriosis-related pain is often understood through patterns involving blood stasis, constrained circulation, inflammation, and nervous system dysregulation. Rather than focusing solely on reproductive anatomy, TCM evaluates how pain, inflammation, and tissue congestion arise from disrupted flow and regulatory imbalance within the body.
Acupuncture has been shown to influence pain signaling, inflammatory mediators, and autonomic nervous system balance, making it a valuable supportive modality in endometriosis care (14). By modulating nervous system activity and improving local circulation, acupuncture may help reduce pain intensity, decrease pelvic tension, and support overall symptom regulation over time.
Within an integrative framework, acupuncture is used to support pain regulation, nervous system balance, circulation, and inflammatory modulation—mechanisms that, when underlying drivers are adequately addressed, can contribute to significant symptom resolution and, in some cases, complete remission of endometriosis.
Next Steps in Endometriosis Care
Living with endometriosis can be physically and emotionally exhausting—especially when symptoms persist despite treatment and answers remain unclear. When care focuses only on symptom control, it can be difficult to understand why progress feels limited or inconsistent.
You may request a free 15-minute consultation with Dr. Martina Sturm to review your health concerns and outline appropriate next steps within a root-cause, systems-based framework.
Frequently Asked Questions About Endometriosis
Can endometriosis cause chronic fatigue?
Yes. Many individuals with endometriosis experience chronic fatigue, even outside the menstrual cycle. This fatigue is thought to result from a combination of persistent inflammatory signaling, immune system activation, disrupted sleep due to pain, and ongoing nervous system stress. Over time, these factors can reduce overall energy availability and increase physical and cognitive exhaustion, even when routine labs appear normal.
Why do hormone tests often appear normal with endometriosis?
Standard hormone tests measure hormone levels circulating in the blood, but endometriosis is primarily a tissue-level signaling disorder. Research shows that endometriotic tissue can demonstrate altered hormone receptor responsiveness—particularly progesterone resistance—despite normal serum estrogen and progesterone levels. This disconnect helps explain why symptoms may persist even when conventional hormone testing does not reveal abnormalities.
Can endometriosis symptoms improve without surgery?
In some cases, symptoms may improve without surgery, particularly when factors such as inflammation, immune dysregulation, and pain signaling are addressed. However, responses vary widely between individuals and depend on lesion location, disease severity, and how long symptoms have been present. Non-surgical approaches do not remove lesions but may influence symptom expression and overall disease burden in certain individuals.
Is endometriosis always progressive?
Endometriosis is considered a chronic condition, but progression is not inevitable. Some individuals experience long periods of relative stability, while others notice gradual symptom expansion over time. Ongoing inflammation, immune dysfunction, and nervous system sensitization are believed to increase the likelihood of progression, which is why early recognition and appropriate evaluation matter—even when symptoms are intermittent.
Why don’t symptoms always match imaging or surgical findings?
Symptom severity in endometriosis does not always correlate with the size or number of visible lesions. Pain and dysfunction are strongly influenced by inflammatory activity, nerve involvement, and central pain sensitization. As a result, individuals with minimal visible disease may experience severe symptoms, while others with extensive lesions may report comparatively mild discomfort.
Still Have Questions?
If the topics above reflect ongoing symptoms or unanswered concerns, a brief conversation can help clarify whether a root-cause approach is appropriate.
Resources
StatPearls Publishing – Endometriosis
Office on Women’s Health – Endometriosis
Human Reproduction Update – Endometriosis: inflammatory mechanisms and fertility implications
Yale Medicine – Endometriosis
Mayo Clinic – Endometriosis: Symptoms and Causes
Endocrine Reviews – Progesterone resistance in endometriosis
Reproductive Sciences – Association between endometriosis and gut microbiota: systematic review and meta-analysis
Frontiers in Immunology – Peritoneal immune microenvironment of endometriosis: role of innate and adaptive immunity
Human Reproduction Update – Genome-wide association studies in endometriosis: systematic review
Environmental Health Perspectives – Phthalate exposure and risk of endometriosis: systematic review and meta-analysis
Journal of Alternative and Complementary Medicine – Comparison of ginger, mefenamic acid, and ibuprofen for dysmenorrhea pain
Gynecological Endocrinology – Melatonin and endometriosis-associated pain: clinical evidence
PLOS ONE – Acupuncture for endometriosis: systematic review and meta-analysis
Gynecological Endocrinology – Efficacy of N-acetylcysteine on endometriosis-related pain and ovarian endometriomas
Phytotherapy Research – Curcumin and endometriosis: anti-inflammatory and antiproliferative effects
Gynecological Endocrinology – Antioxidant therapy with N-acetylcysteine, alpha-lipoic acid, and bromelain in endometriosis-associated pelvic pain