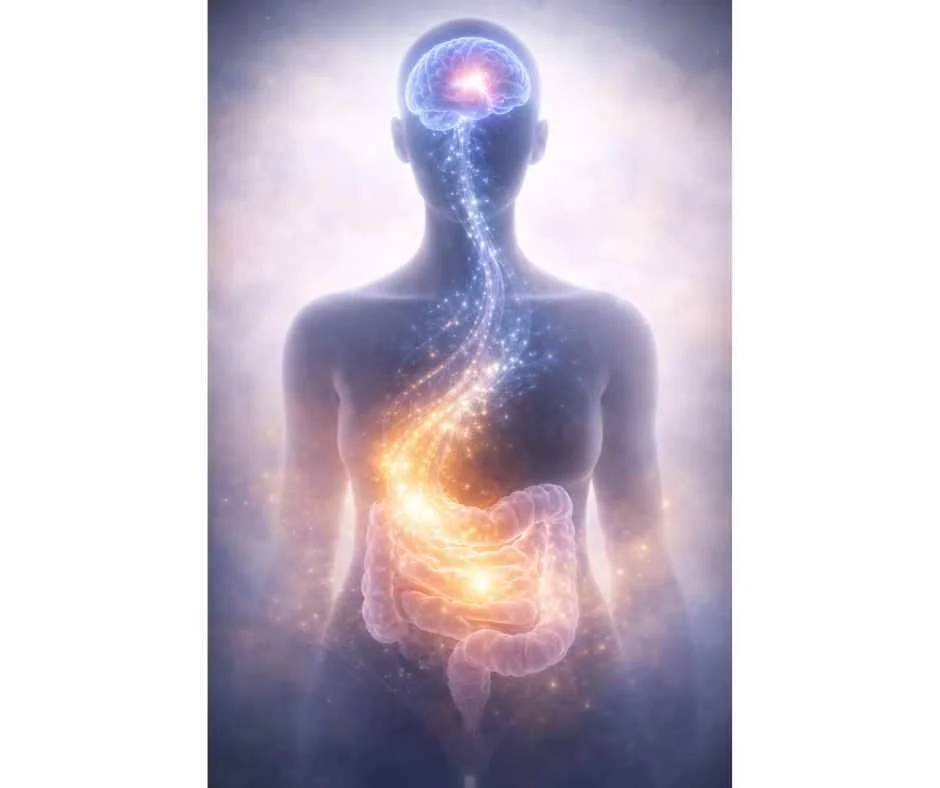
The Gut–Brain Connection: How Gut Health Shapes Mental and Physical Well-Being
Why digestion, stress, mood, and chronic symptoms are biologically linked—and why the gut plays a central role
Hippocrates is often credited with the observation that “all disease begins in the gut.”
Modern research has continued to validate this idea, revealing that gut health plays a central role far beyond digestion alone.
The gut–brain connection describes the constant, two-way communication between the digestive system and the nervous system. This communication influences digestion, inflammation, stress response, and emotional and cognitive regulation.
Research now shows that the majority of signaling along this axis travels from the gut to the brain—not the other way around (1). This helps explain why digestive dysfunction so often overlaps with anxiety, brain fog, fatigue, mood changes, and chronic inflammatory conditions.
Understanding how the gut and brain communicate—and what disrupts that communication—provides a clearer framework for addressing symptoms that don’t respond to isolated or symptom-based treatments.
→ Gut Health & Digestive Restoration
This article discusses the biological foundations of the gut–brain connection, including how gut signaling shapes nervous system function, why disrupted gut health can influence mood and cognition, and how these patterns contribute to complex, overlapping symptoms that are often treated in isolation.
The Gut–Brain Connection Explained
The gut–brain connection is a bidirectional communication pathway between the digestive system and the nervous system. While this relationship was first described by Hippocrates and explored by philosophers such as Aristotle and Plato, modern research has expanded our understanding significantly.
Current evidence shows that changes in gut health can influence a wide range of conditions, including:
Central nervous system disorders such as Parkinson’s disease
Functional gastrointestinal disorders, including IBS and IBD
Neurodevelopmental conditions such as autism
Mental health disorders, including anxiety and depression (2)
Rather than operating as separate systems, the gut and brain function as an integrated network.
At a biological level, this network includes:
The central nervous system (CNS), consisting of the brain and spinal cord
The autonomic nervous system (ANS), including the vagus nerve
The enteric nervous system (ENS), a dense network of neurons embedded within the gut
The hypothalamic axis, which coordinates hormonal signaling throughout the body (3)
Together, these systems regulate digestion, appetite, stress response, immune signaling, and energy balance.
Most people recognize this connection intuitively. Feeling unusually fatigued after a heavy meal, experiencing digestive upset during periods of stress, or noticing your stomach react before conscious hunger sets in are all everyday examples of gut–brain communication at work.
→ Functional & Integrative Medicine
The Brain’s Role in Gut Function
Research consistently shows that gut bacteria influence brain chemistry, affecting emotional regulation, cognition, and stress resilience. Changes in the gut microbiome have been linked to shifts in:
Stress response
Mood regulation
Anxiety and depressive symptoms
Memory and cognitive function
At the same time, signals from the brain directly influence gut motility and digestive efficiency. Under stress, digestion slows. When the nervous system is calm and regulated, digestion becomes more efficient—supporting nutrient absorption and toxin elimination.
The brain also plays a critical role in maintaining the intestinal mucosal barrier, the protective lining where gut bacteria reside. When this balance is disrupted, the environment that supports healthy microbial function begins to break down.
Impaired digestion can alter how nutrients are absorbed and how the microbiome is supported, increasing the likelihood that bacterial fragments cross the intestinal barrier and enter circulation. This process—commonly referred to as intestinal permeability or leaky gut—can activate immune responses and, over time, contribute to inflammatory and autoimmune patterns (3).
When this process persists, symptoms often extend beyond digestion, overlapping with fatigue, joint pain, brain fog, and mood changes—signs that the gut–brain axis is under strain.
The Role of the Gut Microbiome
At its core, the gut–brain connection is the pathway through which signals travel from the gut to the brain.
The gut microbiome refers to the vast community of bacteria living in the intestines that continuously communicates with the nervous system through the neural, immune, and hormonal pathways already described. These signals influence mood, stress response, inflammation, and cognitive function.
The gut microbiome contains tens of trillions of microorganisms and can weigh up to six pounds (8).
Initial microbial colonization begins during birth and early life, but the composition of the microbiome continues to be shaped by factors such as:
Mode of delivery, including cesarean section
Breastfeeding history
Antibiotic exposure
Dietary patterns
Alcohol consumption
NSAID use
Hormonal birth control
When this microbial ecosystem becomes imbalanced—a state known as dysbiosis—the signals sent from the gut to the brain can become distorted, contributing to both digestive and neurological symptoms.
Research shows that altering the composition of gut bacteria can directly change how the brain and body function. Factors that commonly disrupt the microbiome include:
Diets high in sugar, refined carbohydrates, and industrial seed oils
Toxins in food and water
Environmental chemical exposures
Chronic or unmanaged stress
Poor sleep quality
These influences affect the production and signaling of neurotransmitters and hormones that travel from the gut to the brain, shaping brain chemistry and downstream physiological responses.
Importantly, research also demonstrates the reverse. By improving dietary quality, reducing toxic exposure, supporting stress regulation, and prioritizing restorative sleep, it is possible to positively influence the gut microbiome and improve mood, cognitive function, and certain neurodevelopmental conditions (8).
What’s in Your Gut Affects Your Mental Health
Anxiety, depression, and neurodevelopmental conditions such as autism have well-documented links to disruptions within the gut microbiome.
A healthy gut microbiome helps maintain the integrity of the intestinal lining, including the tight junctions that act as a selective barrier between the gut and the bloodstream (11). When this barrier is supported, immune signaling remains regulated and inflammatory responses are kept in check.
When dysbiosis is present, this balance can break down. Microbial imbalance may increase intestinal permeability, allowing bacterial fragments and inflammatory compounds to enter circulation.
This low-grade, chronic inflammation is now understood to play a role in mental health and cognitive changes, as well as systemic conditions such as:
Rheumatoid arthritis
Alzheimer’s disease
Asthma
Allergies
Autism
Parkinson’s disease
Inflammatory bowel diseases (9)
Rather than viewing these conditions in isolation, this research highlights the gut as a central regulator of immune and neurological signaling—helping explain why emotional, cognitive, and physical symptoms often appear together.
How Traditional Chinese Medicine Supports the Gut–Brain Connection
Traditional Chinese Medicine approaches gut–brain health by addressing regulation rather than suppression. Acupuncture, herbal medicine, dietary therapy, and targeted supplementation are used to support balance within the nervous system, digestive system, and immune response. Small, well-directed shifts in gut function can have wide-ranging effects on both physical and mental health.
Traditional Chinese Medicine
Traditional Chinese Medicine is a comprehensive medical system with a long clinical history. It has been widely used in the prevention and treatment of nervous system–related disorders and is centered on supporting homeostasis, or balance, across interconnected systems in the body.
Research increasingly supports the role of TCM in influencing the gut microbiome, particularly in conditions involving stress, inflammation, and mood dysregulation (12). Certain TCM herbal compounds and single herbs have been shown to improve depressive symptoms by helping restore microbial balance and modulate inflammatory signaling—often with fewer side effects than conventional pharmaceutical approaches (13).
Rather than targeting symptoms in isolation, TCM works to improve the underlying terrain that allows the gut and brain to communicate more effectively.
Acupuncture
Acupuncture has demonstrated effectiveness in conditions closely tied to dysbiosis and gut–brain dysfunction, including irritable bowel syndrome. Clinical studies show acupuncture may help:
Improve gut motility
Reduce abdominal pain and discomfort
Modulate immune activity and inflammation
Support signaling along the gut–brain axis (14)
Beyond digestive effects, acupuncture also influences emotional and mental well-being by regulating the autonomic nervous system. In some cases, it has been shown to be as effective as pharmacological therapies for anxiety and depression, with a lower risk of side effects (15).
This dual impact—on both digestion and nervous system regulation—is what makes acupuncture particularly relevant in gut–brain–related conditions.
Diet and Supplements
Diet plays a central role in shaping the gut microbiome. The foods consumed daily can either support microbial diversity and intestinal integrity or contribute to inflammation and imbalance.
Because gut health is highly individual, dietary strategies should be personalized. That said, general principles that tend to support microbiome balance include:
Healthy fats
Grass-fed or finished meats
Wild-caught fish
Fiber-rich foods
Fermented foods
Nuts and seeds
Minimally processed, non-GMO grains
Foods that commonly disrupt gut balance include:
Highly processed or packaged foods
Diets high in added sugar
Artificial additives, colorings, and sweeteners
Hydrogenated and industrial seed oils
Fried foods
Conventionally grown, non-organic crops with higher pesticide exposure
High-quality supplements and herbal formulas can be useful tools for restoring gut function, but they should be selected and monitored under professional guidance to avoid unintended imbalances or interactions (16).
Supporting the Gut–Brain Connection at Denver Sports & Holistic Medicine
The gut, brain, and nervous system function as an integrated whole. When one system is out of balance, symptoms often appear across multiple areas—digestive issues, mood changes, fatigue, inflammation, or stress intolerance.
Addressing these patterns requires a whole-body, systems-based approach. Care at Denver Sports & Holistic Medicine focuses on identifying root contributors to gut–brain dysfunction by integrating functional medicine diagnostics with Traditional Chinese Medicine. This includes evaluating gut microbiome health, nervous system regulation, inflammatory patterns, and metabolic resilience.
Rather than chasing symptoms in isolation, the goal is to restore balance across interconnected systems—supporting digestion, mental clarity, immune function, and long-term health.
If you are experiencing persistent digestive symptoms, mood changes, or stress-related health concerns, a personalized evaluation can help clarify what is driving the imbalance and guide appropriate next steps.
→ Advanced Functional Lab Testing
When Gut–Brain Imbalance Drives Persistent Symptoms
Persistent digestive symptoms, mood changes, fatigue, or stress intolerance often reflect deeper imbalance across the gut, nervous system, and immune response.
Request a free 15-minute consultation with Dr. Martina Sturm. This provides an opportunity to review symptoms, discuss relevant history, and determine whether further evaluation—such as functional gut testing or nervous system support—would be appropriate.
Frequently Asked Questions About the Gut–Brain Connection
What is the gut–brain connection
The gut–brain connection is the two-way communication system linking the digestive tract and the nervous system. It involves the gut microbiome, the enteric nervous system, the autonomic nervous system (including the vagus nerve), immune signaling, and hormonal pathways that collectively influence digestion, inflammation, mood, cognition, and stress response.
Why does gut health affect anxiety and depression
Gut health affects anxiety and depression because gut microbes influence neurotransmitter production, immune signaling, and inflammation. When the microbiome is imbalanced or the intestinal barrier is compromised, inflammatory signals can reach the brain and disrupt emotional regulation, stress resilience, and mood stability.
What is the vagus nerve and why is it important for gut health
The vagus nerve is a primary communication pathway between the gut and the brain. It helps regulate digestion, gut motility, appetite, stress response, and inflammation. Reduced vagal tone is associated with digestive symptoms, heightened stress reactivity, and impaired gut–brain signaling.
Can stress cause digestive symptoms
Yes. Stress activates the sympathetic nervous system and the HPA axis, which can slow digestion, alter gut motility, reduce stomach acid and enzyme production, and shift the gut microbiome. Chronic stress is commonly linked to bloating, constipation, diarrhea, reflux, and food sensitivities.
What is dysbiosis and how does it affect the gut–brain axis
Dysbiosis is an imbalance in the gut microbiome that disrupts normal signaling between the gut and the brain. It can impair gut barrier integrity, increase inflammation, and alter neurotransmitter and hormone signaling, contributing to symptoms such as fatigue, brain fog, mood changes, and digestive discomfort.
What is leaky gut and how does it affect the brain
Leaky gut refers to increased intestinal permeability, allowing inflammatory compounds and bacterial fragments to enter circulation. This can activate immune responses and low-grade inflammation that may influence cognitive function, mood, and systemic symptoms beyond the digestive tract.
How does Traditional Chinese Medicine support the gut–brain connection
Traditional Chinese Medicine supports gut–brain balance by improving regulation across the digestive system, nervous system, and immune response. Approaches such as acupuncture, herbal medicine, dietary therapy, and lifestyle guidance are used to support motility, inflammation balance, stress resilience, and overall homeostasis.
Can acupuncture help gut-related anxiety and stress
Acupuncture may help regulate the autonomic nervous system and improve vagal signaling, which can support both digestive function and stress regulation. Many individuals notice improvements in sleep quality, stress tolerance, and gastrointestinal symptoms when nervous system regulation is addressed.
What are the first steps to improve gut–brain health
Foundational steps include prioritizing consistent sleep, managing stress, eating a whole-food diet, reducing ultra-processed foods and alcohol, and supporting gut barrier integrity and microbial balance when needed. Persistent symptoms often respond best to a personalized, systems-based approach.
Still Have Questions?
If the topics above reflect ongoing symptoms or unanswered concerns, a brief conversation can help clarify whether a root-cause approach is appropriate.
Resources
Nature Reviews Neuroscience – The vagus nerve and bidirectional brain–body communication
Gastroenterology – The microbiota–gut–brain axis: from motility to mood
Nature Reviews Gastroenterology & Hepatology – Gut–brain axis interactions between enteric microbiota and the nervous system
Merck Manual – Overview of the autonomic nervous system
Cleveland Clinic – Autonomic nervous system: function and disorders
Cell – Gut microbe–to–brain signaling mechanisms
National Center for Complementary and Integrative Health – Gut–brain connection: key facts
Biological Psychiatry – Influence of gut microbiota on mood and mental health
Trends in Neurosciences – Modulation of the microbiota–gut–brain axis in depression
Frontiers in Neuroscience – Gut–brain interaction and microbiota-mediated neurogenesis
World Journal of Gastroenterology – Acupuncture and regulation of the gut–brain–microbiota axis in irritable bowel syndrome
World Scientific – Acupuncture effects on gut–brain–microbiota signaling
Rome Foundation – Acupuncture treatment for disorders of gut–brain interaction
Gut Microbes – Dysbiosis and its impact on host physiology
Nutrients – Dietary modulation of the gut–brain axis and mental health