Endocrine Disruptors Explained: How Everyday Toxins Affect Your Hormones
How Endocrine-Disrupting Chemicals Interfere With Hormone Signaling and Long-Term Health
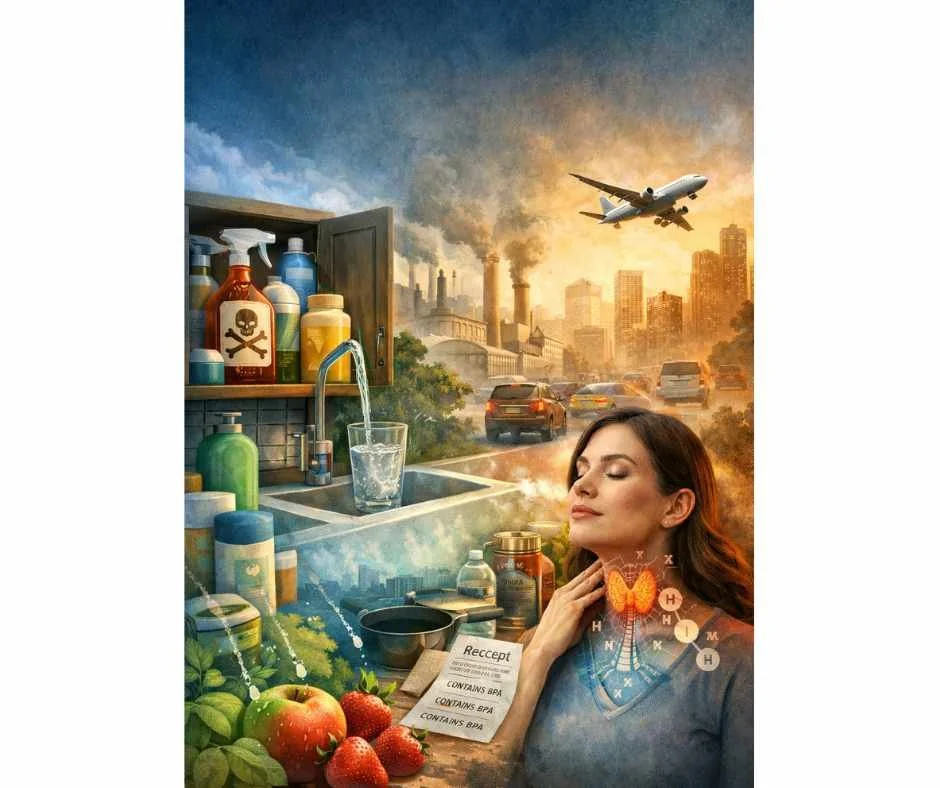
Hormone imbalance is a growing health concern affecting millions of people worldwide. Symptoms such as fatigue, weight gain, infertility, mood changes, thyroid dysfunction, metabolic disturbances, and increased cancer risk are becoming increasingly common across all age groups.
While stress, diet, aging, and lifestyle factors are often discussed as contributors to hormonal imbalance, one significant and frequently overlooked driver is chronic exposure to environmental toxins—specifically endocrine-disrupting chemicals (EDCs).
These chemicals are embedded in everyday life. They are found in plastic bottles, food packaging, personal care products, pesticides, non-stick cookware, household cleaners, flame retardants, and even drinking water. Exposure is often low-dose but continuous, occurring through ingestion, inhalation, and absorption through the skin.
Over time, this cumulative toxic burden can interfere with the body’s finely regulated hormonal signaling systems—often without immediate or obvious symptoms. For many individuals, endocrine disruption develops quietly, contributing to complex, multi-system health issues that are difficult to trace back to a single cause.
This article explains how endocrine-disrupting chemicals affect hormonal health, where these toxins are most commonly encountered, and the practical steps that can reduce exposure and protect endocrine function.
What Are Endocrine-Disrupting Chemicals (EDCs)?
According to the Endocrine Society, endocrine-disrupting chemicals are defined as:
“Exogenous chemicals or mixtures of chemicals that can interfere with any aspect of hormone action.” (1)
How Endocrine-Disrupting Chemicals Enter the Body
EDCs can enter the body through ingestion, inhalation, and skin absorption. Once inside, they may:
Mimic natural hormones such as estrogen, testosterone, or thyroid hormone
Block hormone receptors, preventing normal cellular signaling
Alter hormone production, transport, metabolism, or elimination
How EDCs Interfere With Hormone Signaling
Because hormones act as chemical messengers that regulate metabolism, reproduction, neurological development, immune function, and detoxification, even subtle disruptions can have system-wide consequences.
The Endocrine Society has warned that endocrine-disrupting chemicals are associated with adverse developmental, reproductive, neurological, and immune effects in humans and wildlife (2).
Why Low-Dose, Chronic Exposure Matters
Importantly, EDCs do not always follow traditional toxicology models where “the dose makes the poison.” Research shows that chronic low-dose exposure—particularly during critical windows such as fetal development, childhood, puberty, and midlife hormonal transitions—can exert long-term biological effects, even when exposure levels fall below regulatory safety thresholds.
Common Sources of Endocrine-Disrupting Chemicals
Endocrine-disrupting chemicals are pervasive in modern environments. Exposure typically occurs through daily, repeated contact rather than a single high-dose event. Below are some of the most common and clinically relevant sources.
Endocrine Disruptors in Personal Care Products
Conventional personal care and hygiene products—including soaps, shampoos, lotions, makeup, toothpaste, mouthwash, dental floss, and hand sanitizers—often contain endocrine-disrupting compounds such as synthetic fragrances, triclosan, fluoride, parabens, phthalates, bisphenols, polybrominated diphenyl ethers (PBDEs), aluminum chlorohydrate, and per- and polyfluoroalkyl substances (PFAS), commonly referred to as “forever chemicals.”
Parabens are widely used as preservatives, while phthalates are frequently added to fragrances and plastics to enhance flexibility and scent retention.
Triclosan is an antibacterial agent historically used in soaps, toothpaste, and other hygiene products.
Fluoride is added to toothpaste to prevent tooth decay; however, endocrine disruption is one of its documented adverse effects.
Aluminum salts, commonly used as the active ingredient in antiperspirants, have been strongly linked to breast cancer and hormonal disruption (3).
Endocrine-Disrupting Chemicals in Sunscreen
Chemical sunscreen ingredients such as oxybenzone, octinoxate, and homosalate are readily absorbed through the skin and detectable in the bloodstream. These compounds have been shown to interfere with hormonal signaling and endocrine function (4).
Food Packaging, Plastics, and Thermal Receipts
Bisphenol A (BPA) and its chemical alternatives are commonly found in plastics, food packaging, and can linings, where they can leach into food and beverages—especially when exposed to heat or acidic conditions.
Importantly, “BPA-free” labeling does not eliminate risk, as many BPA substitutes exhibit similar endocrine-disrupting properties. Thermal paper receipts are also coated with BPA, which can be absorbed through the skin within seconds of contact (5).
Pesticides and Herbicides in Food and Water
Agricultural chemicals such as atrazine, glyphosate, dichlorodiphenyltrichloroethane (DDT), and vinclozolin contaminate food and water supplies and are well-documented endocrine disruptors (6).
Endocrine Disruptors in Household Cleaning Products
Many household cleaning agents and detergents contain endocrine-disrupting compounds, including chlorine (bleach), alkylphenols, and perfluorinated compounds, which contribute to cumulative toxic burden through inhalation and skin contact (7).
Food Additives With Hormone-Disrupting Effects
Certain food preservatives, including butylated hydroxyanisole (BHA) and butylated hydroxytoluene (BHT), have demonstrated endocrine-disrupting effects (8).
Endocrine Disruptors in Tap Water
Municipal tap water is a common source of endocrine disruptors, including fluoride, chlorine, glyphosate, atrazine, arsenic, and water disinfection byproducts (DBPs) such as trihalomethanes (THMs) and haloacetic acids (HAAs) (9).
Chlorine and Bromine Exposure From Pools and Hot Tubs
Chlorine and bromine—the most commonly used disinfectants in pools and hot tubs—are known endocrine disruptors. These halogens can displace iodine, a critical element required for healthy thyroid function and breast tissue integrity.
Non-Stick Cookware and PFAS Exposure
Non-stick cookware coated with polytetrafluoroethylene (PTFE), commonly known as Teflon, can release toxic fumes and chemicals when heated to high temperatures. These compounds are considered endocrine disruptors and may leach into food during cooking (10).
Heavy Metals as Endocrine Disruptors
Several heavy metals—including lead (Pb), mercury (Hg), arsenic (As), cadmium (Cd), and nickel (Ni)—are well-established endocrine disruptors.
Although less common in gasoline and paint today, lead remains ubiquitous in batteries, glass, coatings, pesticides, and plumbing materials.
Mercury exposure most commonly occurs through vaccines, older dental amalgams, and consumption of large predatory fish such as tuna, swordfish, marlin, and sea bass.
Cadmium exposure arises primarily from tobacco smoke (including secondhand exposure), environmental pollution, and dietary sources.
Arsenic, a highly toxic level-1 carcinogen, is most commonly encountered through contaminated drinking water, with additional exposure from processed foods and polluted air (11).
Flame Retardants and Indoor Air Exposure
Flame retardants such as polybrominated diphenyl ethers (PBDEs) have been widely used in clothing, furniture, building materials, baby products, and electronics to slow ignition and fire spread.
As these treated products age, PBDEs volatilize and accumulate in indoor air and household dust, increasing chronic inhalation and ingestion exposure (12).
Endocrine Disruptors in Menstrual Products
Conventional disposable menstrual products, including pads and tampons, may contain phthalates, bisphenols, pesticides, and other endocrine-disrupting chemicals, posing a direct exposure risk through highly absorptive tissue.
Synthetic Fragrances and Scented Products
Candles, perfumes, room fresheners, dryer sheets, and other scented products often contain undisclosed chemicals under the umbrella term “fragrance.” Manufacturers are not required to list individual fragrance components, many of which are known endocrine disruptors.
How Endocrine-Disrupting Chemicals Affect Hormonal Health
Hormone Mimicry and Receptor Interference
Endocrine-disrupting chemicals affect hormonal health by mimicking natural hormones, blocking hormone receptors, or altering receptor sensitivity. Some compounds bind to estrogen, androgen, or thyroid hormone receptors, triggering inappropriate signaling, while others prevent normal hormones from binding and exerting their effects.
Because hormone receptors regulate gene expression, metabolism, growth, reproduction, and immune activity, even subtle receptor-level interference can produce wide-ranging physiological effects.
Disruption of Hormone Production, Transport, and Metabolism
Beyond receptor effects, endocrine-disrupting chemicals interfere with hormone synthesis, conversion, transport, and clearance. These disruptions can alter enzyme activity involved in hormone production, impair liver-based hormone metabolism, or affect hormone-binding proteins that regulate hormone availability at the tissue level.
As a result, circulating hormone levels may appear normal on standard testing while tissue-level signaling remains impaired.
System-Wide Effects on Hormonal Networks
Rather than affecting a single hormone in isolation, endocrine-disrupting chemicals disrupt interconnected hormonal networks. Alterations in one pathway often cascade into others, influencing reproductive function, metabolic regulation, neurological signaling, immune balance, thyroid activity, and cancer-related gene expression.
This systems-level disruption helps explain why chronic exposure to endocrine-disrupting chemicals is associated with complex, multi-system health patterns rather than isolated hormonal symptoms.
Health Effects of Endocrine Disruption
Endocrine-disrupting chemicals do not affect hormonal health in isolation. By interfering with hormone signaling, metabolism, and receptor activity, these compounds can influence multiple physiological systems simultaneously. The health effects associated with endocrine disruption often reflect this systems-level interference, with manifestations that vary based on timing, duration, and cumulative exposure.
Reproductive and Fertility Effects
Endocrine-disrupting chemical exposure is associated with impaired reproductive function, including polycystic ovary syndrome (PCOS) and endometriosis in women, as well as reduced sperm quality and altered fertility parameters in men (13). These effects reflect disruption of sex hormone signaling, steroidogenesis, and reproductive tissue development.
Developmental and Puberty-Related Effects
Exposure to endocrine disruptors during critical developmental windows has been linked to developmental delays, earlier onset of puberty, and behavioral and cognitive challenges in children (14). These effects are particularly concerning because hormonal signaling plays a central role in growth, neurodevelopment, and sexual maturation.
Metabolic Dysfunction and Insulin Resistance
Endocrine disruptors contribute to obesity, insulin resistance, type 2 diabetes, and metabolic syndrome by altering adipocyte signaling, appetite regulation, and glucose metabolism (15). These compounds are often referred to as “obesogens” due to their ability to promote fat storage and metabolic dysregulation independent of caloric intake.
Neurological and Cognitive Effects
Certain endocrine-disrupting chemicals interfere with neural signaling, synapse formation, and neurotransmitter regulation. These disruptions have been implicated in the development of neurological and neurobehavioral disorders, particularly when exposure occurs during early brain development (16).
Immune Dysregulation and Inflammation
Endocrine-disrupting chemicals influence immune system development and regulatory balance, increasing susceptibility to immune dysregulation, chronic inflammation, and altered immune responses (17). Hormonal signaling plays a key role in immune tolerance, making endocrine disruption a relevant factor in inflammatory and autoimmune patterns.
Thyroid Dysfunction and Autoimmune Risk
Many endocrine disruptors interfere with thyroid hormone synthesis, transport, conversion, and receptor binding. These disruptions are associated with hypothyroidism, autoimmune thyroid disease, and broader metabolic disturbances linked to impaired thyroid signaling (18).
Hormone-Sensitive Cancer Risk
Long-term exposure to endocrine-disrupting chemicals is associated with an increased risk of hormone-sensitive cancers, including breast and prostate cancer. These risks are linked to hormone-mimicking activity, altered gene expression, and disruption of normal cell signaling pathways involved in growth and differentiation (19, 20).
How to Reduce Exposure to Endocrine-Disrupting Chemicals
Reducing exposure to endocrine-disrupting chemicals is a foundational strategy for protecting long-term hormonal regulation. The following approaches focus on practical, sustainable ways to lower daily toxic burden across common environmental sources.
Choosing Cleaner Personal Care and Cleaning Products
Opt for personal care and household cleaning products that are free from synthetic fragrances, parabens, phthalates, triclosan, PFAS, and other known endocrine disruptors. Even small daily changes can significantly reduce cumulative exposure over time.
Reducing Oral and Dental Product Exposure
Use fluoride-free toothpaste and natural dental floss that is not coated with PFAS (“forever chemicals”). A simple non-toxic mouthwash can be made using baking soda with tea tree and peppermint essential oils.
Avoiding Plastics and Printed Receipts
Plastics used for food storage, utensils, cans, plastic wrap, zip-top bags, and takeaway containers—particularly those with recycling codes 3 and 7—often contain bisphenols that can leach into food, especially when heated or exposed to acidic conditions.
Choose glass or stainless steel containers whenever possible, buy foods with minimal packaging, and opt for glass or Tetra Pak when available.
Avoid handling printed receipts when possible, or request digital receipts, as bisphenols are rapidly absorbed through the skin.
Filtering Drinking and Cooking Water
Tap water commonly contains endocrine disruptors such as phthalates, bisphenols, atrazine, pharmaceutical residues, fluoride, and other halogens.
Use a high-quality water filtration system capable of removing fluoride, chlorine, and chemical contaminants. Refrigerator filters are not sufficient. Reverse osmosis or high-quality activated carbon systems are more effective.
Always cook with filtered water.
Limiting Processed and Packaged Foods
Processed foods often contain preservatives, food dyes, flavor enhancers listed as “natural flavors,” and brominated additives that act as endocrine disruptors.
Avoid foods containing brominated vegetable oils (BVOs) and other bromine-based additives. Prioritize whole, unprocessed foods such as vegetables, fruits, healthy fats, and clean protein sources.
Choosing Organic and Regeneratively Sourced Foods
Organic produce is grown without synthetic pesticides and herbicides, reducing exposure to common endocrine disruptors. Avoid genetically modified foods, which are frequently treated with glyphosate-based herbicides.
While organic is the best option, cross-contamination can still occur. Soaking produce in 2 cups of water with 1 teaspoon of baking soda for 15 minutes can remove most remaining pesticide residues (21).
Avoid meat, dairy, and eggs from concentrated animal feeding operations (CAFOs), where animals and feed are exposed to antibiotics, hormones, and industrial chemicals.
Choose regeneratively farmed meats, pasture-raised eggs, and raw dairy when appropriate. Opt for wild-caught fish—particularly smaller species such as salmon, sardines, anchovies, mackerel, and herring—which contain lower levels of mercury, heavy metals, and microplastics.
Avoiding Non-Stick Cookware
Cookware coated with polytetrafluoroethylene (PTFE), commonly known as Teflon, can release toxic fumes and leach endocrine-disrupting chemicals into food when heated.
Choose safer alternatives such as stainless steel, cast iron, or ceramic cookware (22).
Reducing Flame Retardant Exposure at Home
When purchasing furniture, carpets, electronics, or textiles, check labels for brominated flame retardants. Choose products made from organic cotton, wool, linen, or silk instead of synthetic materials.
Improving Indoor Air Quality and Ventilation
Ensure regular ventilation to reduce indoor off-gassing from treated furniture and building materials. Maintain a dust-free environment using HEPA-filter vacuums and air purifiers. Wet mopping and damp dusting are preferable to dry methods that redistribute toxins.
Limiting Chlorine Exposure in Water
Limit time spent in chlorinated pools and hot tubs when possible. Shower immediately afterward to reduce skin absorption and inhalation of disinfection byproducts. Installing a shower filter can significantly reduce daily chlorine exposure.
Choosing Mineral-Based Sunscreens
Choose mineral-based sunscreens containing zinc oxide or titanium dioxide rather than chemical sunscreens. When outdoors for extended periods, alternate sun exposure with shade or wear sun-protective clothing.
Reading Labels to Identify Hidden Endocrine Disruptors
Many endocrine disruptors are hidden in everyday products. Learning to read labels and choosing cleaner alternatives can dramatically reduce toxic burden. Resources such as the Environmental Working Group can help identify safer product options.
Supporting Detoxification Pathways Safely
First and foremost, reducing exposure to endocrine-disrupting chemicals is the most important step in protecting hormonal health. Detoxification is not about aggressively “cleansing” the body—it is about supporting the organs and systems responsible for processing, transforming, and eliminating toxins safely.
When detox pathways are supported appropriately, the body is better equipped to handle ongoing environmental exposures while minimizing hormonal disruption.
Nutrient-Dense Diet and Detox Cofactors
A nutrient-dense diet provides the biochemical building blocks required for detoxification. Vitamins, minerals, antioxidants, amino acids, and phytonutrients are essential for liver enzyme function, antioxidant defense, and hormone metabolism.
Focus on whole foods including vegetables, fruits, clean protein sources, and healthy fats to support the body’s natural detoxification capacity.
Hydration and Renal Elimination
Adequate hydration supports kidney function and the elimination of water-soluble toxins through urine. Drinking clean, filtered water throughout the day helps maintain efficient detox pathways and prevents toxin reabsorption.
Herbal Support for Liver and Bile Flow
Certain herbs can gently support detoxification, particularly liver and bile function. Teas such as dandelion root, milk thistle, and green tea provide antioxidant and hepatoprotective compounds that assist the body’s natural detox processes.
Movement, Lymphatic Flow, and Circulation
Physical activity improves circulation, stimulates lymphatic flow, and supports metabolic detoxification. Movement also promotes sweating, which serves as an auxiliary elimination pathway for certain toxins.
A balanced approach—including cardiovascular exercise, strength training, and mobility work—supports detoxification without overstressing the system.
Sauna Therapy and Sweating
Sauna therapy promotes sweating and circulation, supporting toxin elimination through the skin. When used appropriately, sauna use may help reduce overall toxic burden and support metabolic and cardiovascular health.
Sauna therapy should be individualized, especially for those with adrenal, cardiovascular, or chronic illness concerns.
Dry Brushing and Lymphatic Support
Dry brushing can stimulate lymphatic flow and exfoliation, supporting one of the body’s most overlooked detox pathways. Gentle, consistent lymphatic support can aid toxin transport without forcing elimination.
Detoxifying Baths and Mineral Support
Soaking in baths with Epsom salts, baking soda, or apple cider vinegar may support relaxation and mineral replenishment while assisting mild detoxification through the skin. These practices should be supportive—not aggressive—and used based on individual tolerance.
Liver Support for Hormone Metabolism
The liver is the primary organ responsible for detoxification and hormone metabolism. Supporting liver function is foundational when addressing endocrine disruption.
Nutrients and botanicals such as milk thistle, dandelion root, and N-acetylcysteine (NAC) may help support glutathione production, phase I and phase II detoxification pathways, and overall liver resilience.
This type of support is best guided by individualized assessment rather than generalized protocols.
Why Detoxification Should Be Personalized
Assessing Detox Capacity and Toxic Load
While foundational lifestyle strategies are beneficial, more structured detoxification should never be approached as a one-size-fits-all program. Individual detox capacity varies based on genetics, nutrient status, gut integrity, liver function, renal clearance, lymphatic flow, and total toxic burden.
Without understanding these variables, detoxification efforts may be ineffective or counterproductive.
Avoiding Detox Reactions and Hormonal Worsening
Mobilizing toxins without adequate drainage, liver support, or elimination capacity can worsen symptoms and disrupt hormonal balance. Common consequences include fatigue, headaches, mood changes, sleep disruption, digestive symptoms, and exacerbation of hormone-related complaints.
A comprehensive, systems-based approach may include:
Evaluating detoxification capacity
Identifying specific environmental or chemical exposures
Supporting gut, liver, lymphatic, and kidney pathways
Monitoring hormone, metabolic, and inflammatory markers
This sequencing helps ensure toxins are processed and eliminated safely rather than redistributed within the body.
When Functional Lab Testing Is Appropriate
When symptoms are persistent, exposure history is complex, or previous detox efforts have worsened symptoms, targeted assessment becomes essential. Functional testing can help clarify toxic load, detox capacity, and physiological readiness for more structured interventions.
→ Advanced Functional Lab Testing
Before beginning a more intensive detoxification program, working with a qualified functional medicine practitioner helps ensure strategies are safe, individualized, and aligned with the body’s ability to regulate and recover.
Protecting Hormonal Health in a High-Toxicity Environment
Awareness of the impact of endocrine-disrupting chemicals (EDCs) on hormonal health is an essential first step toward long-term wellbeing. Minimizing exposure through informed choices in personal care products, food sourcing, water quality, and household materials can meaningfully reduce toxic burden and support hormonal balance.
Incorporating supportive detoxification strategies—such as a nutrient-rich diet, adequate hydration, regular movement, and targeted liver support—helps the body process and eliminate environmental toxins more effectively. Over time, these foundational practices can reduce cumulative exposure and mitigate the downstream effects of endocrine disruption.
Importantly, meaningful improvement does not require perfection. Small, consistent lifestyle adjustments can produce measurable benefits in hormonal resilience and overall physiological regulation.
When symptoms such as hormone imbalance, metabolic dysfunction, thyroid concerns, fertility challenges, or unexplained chronic symptoms persist, a personalized and systems-based approach is often necessary to identify contributing exposures and support recovery.
→ Detoxification & Environmental Medicine
You may request a free 15-minute consultation with Dr. Martina Sturm to review your health concerns and outline appropriate next steps within a root-cause, systems-based framework.
A targeted, individualized plan can help address environmental exposures, support detoxification pathways, and restore hormonal regulation in a sustainable and clinically appropriate manner.
Frequently Asked Questions About Endocrine-Disrupting Chemicals (EDCs)
What are endocrine-disrupting chemicals (EDCs)?
Endocrine-disrupting chemicals (EDCs) are environmental compounds that interfere with hormone production, signaling, transport, or metabolism. They may mimic natural hormones, block hormone receptors, or alter how hormones are broken down and eliminated, contributing to hormonal imbalance and downstream health issues such as thyroid dysfunction, infertility, metabolic disorders, and hormone-sensitive cancers.
Where are EDCs most commonly found?
EDCs are found in many everyday products and environments, including personal care products, household cleaners, food packaging, tap water, non-stick cookware, pesticides and herbicides, menstrual products, scented candles, air fresheners, and printed receipts.
How do EDCs affect hormone health?
EDCs disrupt hormonal communication throughout the body. This interference can contribute to reproductive dysfunction, thyroid imbalance, early puberty, insulin resistance, metabolic disorders, neurological effects, immune dysregulation, and an increased risk of hormone-related cancers such as breast and prostate cancer.
What health issues are linked to long-term EDC exposure?
Chronic exposure to endocrine disruptors has been associated with infertility, PCOS, endometriosis, early puberty in children, obesity, type 2 diabetes, thyroid disorders, autoimmune conditions, neurological dysfunction, and impaired immune regulation.
How can I reduce my exposure to EDCs at home?
Reducing exposure starts with practical daily changes, such as switching to fragrance-free personal care and cleaning products, using glass or stainless steel food containers, filtering drinking and cooking water, choosing organic foods when possible, and avoiding synthetic fragrances, processed foods, and non-stick cookware.
Are organic foods free from endocrine disruptors?
Organic foods are grown without synthetic pesticides and herbicides, significantly reducing exposure to many endocrine disruptors. However, cross-contamination can still occur. Washing and soaking produce—such as using a baking soda solution—can further reduce residual pesticide exposure.
Can endocrine disruptors be completely eliminated from the body?
Complete elimination of all endocrine disruptors is unlikely due to ongoing environmental exposure. However, the body has natural detoxification pathways that can be supported through proper nutrition, hydration, regular movement, sauna use when appropriate, and liver-supportive nutrients and herbs. Detoxification is safest and most effective when individualized and guided by a qualified practitioner.
What type of water filter helps reduce EDC exposure?
High-quality filtration systems such as reverse osmosis or well-designed activated carbon filters are most effective for reducing endocrine disruptors in water. Standard refrigerator filters are not sufficient to remove contaminants such as fluoride, chlorine, glyphosate, or pharmaceutical residues.
Are there safer alternatives to chemical sunscreens?
Yes. Mineral-based sunscreens containing zinc oxide or titanium dioxide provide effective sun protection without the endocrine-disrupting effects associated with chemical sunscreen ingredients such as oxybenzone and octinoxate.
When should detoxification be done with professional guidance?
If you are experiencing symptoms of hormonal imbalance, fertility challenges, chronic fatigue, thyroid issues, or have known or suspected high toxic exposure, professional guidance is strongly recommended. Working with a qualified functional medicine practitioner helps ensure detoxification is safe, personalized, and supportive rather than disruptive.
Still Have Questions?
If the topics above reflect ongoing symptoms or unanswered concerns, a brief conversation can help clarify whether a root-cause approach is appropriate.
Resources
Endocrine Reviews – Endocrine-disrupting chemicals and public health protection: principles from the Endocrine Society
National Institute of Environmental Health Sciences – Endocrine disruptors and human health
Environmental Health Perspectives – Aluminum compounds and estrogen receptor signaling mechanisms
International Journal of Environmental Research and Public Health – Sunscreen ingredients and endocrine-related health effects: systematic review
Nature Reviews Endocrinology – Bisphenol A and endocrine disruption in carcinogenesis and therapy response
Toxicology Letters – Endocrine-disrupting pesticide exposure and hormonal interference mechanisms
Environmental Science & Technology – Mixture toxicity of endocrine-disrupting chemicals in household products
Food and Chemical Toxicology – Endocrine-disrupting effects of butylated hydroxyanisole (BHA)
Water Research – Endocrine disruptors in water and reproductive system effects
Environment International – Endocrine-disrupting potential of per- and polyfluoroalkyl substances (PFAS)
Toxicology and Applied Pharmacology – Endocrine-disrupting heavy metals and human health impacts
Environmental Health Perspectives – Endocrine-active flame retardants: exposure pathways and mechanisms
Hormones and Behavior – Disruption of sex hormone activity by environmental endocrine disruptors
Environmental Research – Environmental endocrine disruptor exposure and child development outcomes
Endocrine Reviews – Metabolic syndrome and endocrine-disrupting chemicals
Neuroscience & Biobehavioral Reviews – Endocrine disruptors and neural development and neurologic disease risk
Frontiers in Immunology – Immune system mediation of endocrine disruptor effects on metabolic health
Thyroid – Endocrine-disrupting chemicals and thyroid hormone signaling
Trends in Endocrinology & Metabolism – Chemical endocrine disruptors and global endocrine system effects
Neurotoxicology – Behavioral and neuroendocrine effects of endocrine-disrupting chemicals
Journal of Agricultural and Food Chemistry – Removal of pesticide residues from produce using commercial and household washing agents
Environmental Health Perspectives – Toxicological concerns related to PTFE-coated non-stick cookware