A Holistic Approach to Sleep Apnea: How Functional Medicine and Acupuncture Can Help You Breathe Easier
Understanding airway dysfunction, standard medical treatment, and integrative strategies that support breathing, sleep quality, inflammation control, and whole-body regulation
Sleep apnea is a common but often underrecognized sleep-related breathing disorder that affects millions of adults worldwide. Far more than a problem of snoring or poor sleep, sleep apnea involves repeated disruptions in airflow during the night that place ongoing physiological stress on the cardiovascular system, brain, metabolic pathways, and nervous system (1).
When breathing repeatedly pauses or becomes restricted during sleep, oxygen levels fluctuate and the body is repeatedly pushed into a stress response. Over time, this pattern has been associated with excessive daytime fatigue, impaired concentration, mood changes, metabolic dysfunction, elevated cardiovascular risk, and reduced overall quality of life. Many individuals live with symptoms for years before receiving a formal diagnosis (2).
Conventional medical care for sleep apnea appropriately prioritizes maintaining adequate airflow during sleep through interventions such as positive airway pressure therapy, oral appliances, or—when indicated—surgical approaches. These treatments are often essential for protecting long-term health and reducing immediate risk. However, they primarily focus on preventing airway collapse rather than examining why breathing dysregulation and airway instability developed in the first place (3).
A holistic, integrative approach to sleep apnea expands this perspective by identifying and addressing contributing factors such as airway mechanics, inflammation, metabolic health, hormonal balance, nervous system regulation, and lifestyle influences that affect breathing patterns during sleep (4).
This article explores how sleep apnea develops, why its effects extend far beyond disrupted sleep, and how functional medicine and acupuncture can be integrated with conventional treatment to support airway stability, reduce physiological stress, and promote more resilient, whole-body regulation over time (5).
What Is Sleep Apnea?
Sleep apnea is a sleep-related breathing disorder defined by repeated reductions or complete pauses in airflow during sleep, resulting in intermittent hypoxia and fragmented sleep architecture (6). These events can occur dozens—or even hundreds—of times per night and often happen without the individual’s conscious awareness.
Rather than being a simple mechanical issue, sleep apnea reflects instability in airway structure, neuromuscular control, and respiratory regulation. Recurrent oxygen fluctuations and sleep disruption activate stress pathways and interfere with the body’s ability to cycle through restorative stages of sleep.
Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea is the most common form of sleep apnea. It occurs when the muscles of the throat and upper airway relax excessively during sleep, allowing the airway to narrow or collapse despite continued respiratory effort (7).
When airflow becomes restricted or blocked, the brain briefly arouses the body to restore breathing. These repeated micro-arousals prevent sustained deep sleep and contribute to ongoing sympathetic nervous system activation, even when the individual does not fully wake or recall the events.
OSA is often influenced by factors such as airway anatomy, nasal obstruction, excess tissue around the neck, inflammation, and reduced upper airway muscle tone.
Central Sleep Apnea (CSA)
Central sleep apnea is less common and arises from impaired signaling between the brain and the muscles responsible for breathing. In this form, airflow pauses occur because respiratory drive is temporarily reduced or absent, rather than due to physical airway collapse (8).
CSA is more frequently associated with underlying neurological conditions, cardiovascular disease, or dysregulation of central respiratory control mechanisms. Because the airway itself may remain open, treatment considerations differ from those used for obstructive sleep apnea.
Mixed and Complex Sleep Apnea
Some individuals experience mixed or complex sleep apnea, which includes features of both obstructive and central mechanisms. In these cases, airway collapse and impaired respiratory signaling may coexist or emerge at different points during sleep (9).
Why Identifying the Type of Sleep Apnea Matters
Regardless of type, untreated sleep apnea disrupts normal sleep cycles, activates stress physiology, and places ongoing strain on cardiovascular, metabolic, and neurological systems over time (10).
Accurately identifying the form and severity of sleep apnea is essential because it informs:
Selection of appropriate medical therapy
Anticipated response to treatment
Which supportive integrative strategies may be most effective
This diagnostic clarity provides the foundation for combining standard medical management with targeted functional and integrative approaches later in care.
Why Sleep Apnea Affects More Than Sleep
Sleep apnea is often discussed in terms of disrupted rest or loud snoring, but its effects extend far beyond sleep quality alone. Repeated breathing interruptions trigger intermittent hypoxia, sympathetic nervous system activation, and fragmented sleep architecture, creating cumulative physiological stress that affects multiple organ systems over time (11).
Because these disruptions occur night after night—often without conscious awareness—the downstream consequences tend to develop gradually, making sleep apnea a frequent but underrecognized driver of chronic disease.
Cardiovascular Effects of Sleep Apnea
Intermittent hypoxia and repeated arousals activate stress pathways that place sustained strain on the cardiovascular system. Over time, this can contribute to:
Elevated blood pressure and loss of normal nocturnal dipping
Endothelial dysfunction and impaired vascular signaling
Cardiac rhythm disturbances
Increased risk of coronary artery disease and stroke (12)
These cardiovascular effects help explain why untreated sleep apnea is strongly associated with long-term cardiovascular morbidity.
Metabolic Dysfunction and Insulin Resistance
Sleep apnea disrupts metabolic regulation through a combination of hypoxia-driven inflammation, hormonal dysregulation, and altered autonomic balance. Common metabolic consequences include:
Insulin resistance and impaired glucose metabolism
Increased fat storage and reduced metabolic flexibility
Higher risk of type 2 diabetes and metabolic syndrome (13)
These effects may occur independently of body weight, meaning sleep apnea can worsen metabolic health even in individuals who are not obese.
Neurological and Cognitive Consequences
Fragmented sleep and repeated oxygen fluctuations impair normal brain recovery processes. Over time, individuals with sleep apnea may experience:
Brain fog and reduced concentration
Memory impairment
Mood changes, including anxiety and depression
Increased risk of workplace and motor vehicle accidents (14)
These cognitive and emotional effects are often among the earliest—but least recognized—manifestations of sleep-disordered breathing.
Hormonal and Immune Dysregulation
Sleep plays a central role in hormonal signaling and immune regulation. When sleep architecture is repeatedly disrupted, downstream effects may include:
Altered cortisol rhythms and stress hormone imbalance
Interference with thyroid and sex hormone signaling
Chronic low-grade inflammatory activation
Impaired immune regulation and recovery capacity (15)
Over time, this dysregulation can amplify inflammation, slow healing, and increase vulnerability to other chronic conditions.
Why Sleep Apnea Is a Systemic Condition
Because these effects develop gradually, sleep apnea often remains undiagnosed for years—frequently until secondary health concerns such as hypertension, metabolic disease, mood disorders, or cardiovascular events emerge.
Recognizing sleep apnea as a systemic condition rather than a sleep issue alone underscores the importance of timely diagnosis, appropriate medical treatment, and supportive integrative strategies that address the broader physiological impact of sleep-disordered breathing (16).
Conventional Medical Treatments for Sleep Apnea
Conventional medical treatment for sleep apnea focuses on maintaining adequate airflow during sleep to prevent oxygen desaturation and reduce strain on cardiovascular and nervous system function. The most appropriate therapy depends on the type and severity of sleep apnea, airway anatomy, underlying medical conditions, and individual tolerance (17).
These treatments play a critical role in reducing immediate health risks and protecting long-term outcomes, particularly in moderate to severe disease.
Positive Airway Pressure (PAP) Therapy
Positive airway pressure therapy is considered the cornerstone of treatment for moderate to severe obstructive sleep apnea.
Continuous Positive Airway Pressure (CPAP)
CPAP delivers a constant level of pressurized air to keep the upper airway open during sleep. It is widely regarded as first-line therapy due to its effectiveness in reducing apnea events and improving oxygenation when used consistently. Common barriers to adherence include mask discomfort, nasal congestion, dryness, or difficulty tolerating pressure (18).
Bilevel Positive Airway Pressure (BiPAP)
BiPAP provides higher pressure during inhalation and lower pressure during exhalation, which may improve comfort for individuals who struggle with standard CPAP. It is often used in complex or mixed sleep apnea cases, or when higher pressures are required (19).
Oral Appliance Therapy
Oral appliances are typically prescribed for individuals with mild to moderate obstructive sleep apnea or for those who are unable to tolerate PAP therapy.
Common devices include:
Mandibular advancement devices that reposition the lower jaw forward
Tongue-retaining devices designed to reduce airway collapse
These appliances can reduce apnea severity and snoring in selected patients but are generally less effective in more severe cases or when airway obstruction occurs at multiple anatomical levels (20).
Surgical Interventions for Sleep Apnea
Surgical treatment may be considered when structural airway obstruction is significant or when other therapies have failed. Procedures are highly individualized and require careful evaluation by experienced specialists.
Examples include:
Uvulopalatopharyngoplasty (UPPP)
Genioglossus advancement
Maxillomandibular advancement (MMA)
Hypoglossal nerve stimulation
Tracheostomy, reserved for severe or life-threatening cases (21)
Surgical interventions may improve airway anatomy and reduce obstruction, but outcomes vary and long-term success depends on patient selection and underlying physiology.
Limitations of a Symptom-Focused Approach
While conventional therapies are often essential for safety and risk reduction, they primarily address airway patency rather than the broader physiological factors that contribute to sleep-disordered breathing.
Inflammation, metabolic dysfunction, neuromuscular control, hormonal balance, and nervous system regulation can all influence airway stability and treatment response. When these contributors are not addressed, symptom control may be incomplete or difficult to sustain.
This creates a clear role for integrative and functional medicine strategies to complement standard treatment—supporting airway physiology, metabolic health, inflammation regulation, and nervous system balance alongside evidence-based medical care (22).
Airway Physiology and the Role of Nasal Breathing
Sleep apnea does not occur in isolation. It develops within the broader context of airway anatomy, breathing patterns, and neuromuscular regulation—all of which influence how stable the upper airway remains during sleep.
One of the most important, and often overlooked, contributors to sleep-disordered breathing is how a person breathes while awake, as daytime breathing patterns strongly influence nighttime airway behavior.
How Breathing Patterns Influence Airway Stability
Healthy breathing occurs primarily through the nose. Nasal breathing supports several mechanisms essential for airway stability, including:
Proper tongue posture and upper airway positioning
Balanced muscle tone in the jaw, throat, and neck
More efficient oxygen exchange
Regulation of nitric oxide, which supports vascular function and airway dilation (23)
When nasal breathing is impaired—due to chronic congestion, allergies, structural restriction, or long-standing habit—many individuals default to mouth breathing, particularly during sleep.
→ The Power of Nasal Breathing: How It Improves Oral & Overall Health
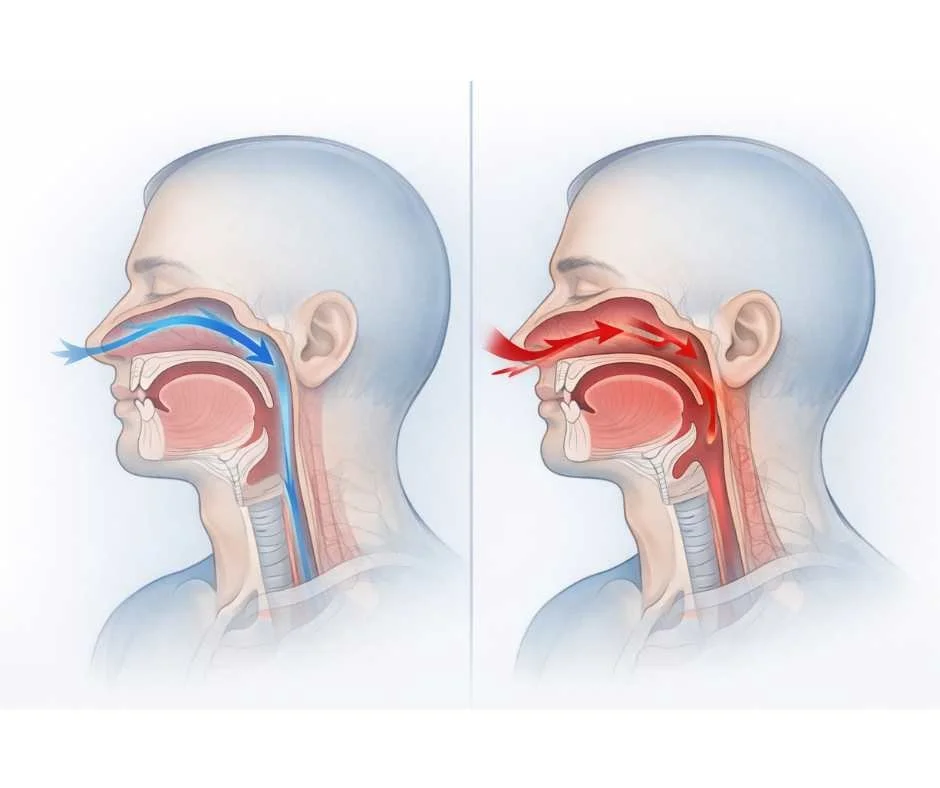
Mouth Breathing and Airway Collapse
Chronic mouth breathing alters airway mechanics in ways that increase vulnerability to obstruction:
The tongue rests lower and farther back, narrowing the airway
Upper airway muscles are more prone to collapse during sleep
Airway resistance increases
Sleep becomes lighter and more fragmented (24)
Over time, these changes can contribute to snoring, airway instability, and the development or worsening of obstructive sleep apnea—especially when combined with inflammation, weight gain, or reduced neuromuscular tone.
Importantly, sleep-disordered breathing often begins years before obstructive sleep apnea is formally diagnosed, frequently rooted in impaired nasal airflow and dysfunctional breathing patterns rather than overt airway collapse alone.
Why Airway Physiology Matters in Sleep Apnea Care
Understanding airway physiology helps explain why effective sleep apnea care requires more than simply forcing air through a narrowed passage. While positive airway pressure devices are often essential for maintaining safety, long-term outcomes may also depend on supporting:
Nasal airflow and breathing mechanics
Upper airway muscle tone
Nervous system regulation
Inflammatory balance
This airway-first perspective provides a critical foundation for integrative strategies that support conventional treatment by improving airway stability and physiologic resilience rather than attempting to replace medical therapy.
→ Acupuncture & Nervous System Regulation
By addressing breathing patterns, neuromuscular coordination, and autonomic balance, integrative approaches can help reduce the physiological drivers that contribute to airway instability during sleep.
A Functional Medicine Perspective on Sleep Apnea
From a functional medicine perspective, sleep apnea is understood as a condition shaped by the interaction of multiple physiological systems rather than a single structural abnormality. While maintaining airway patency during sleep is essential for safety, understanding why airway instability develops can help guide supportive strategies that improve physiological resilience and long-term outcomes.
This perspective focuses on identifying upstream contributors that influence airway tone, neuromuscular coordination, inflammation, and respiratory regulation.
Key Contributors That Can Worsen Sleep Apnea
Metabolic Health and Insulin Resistance
Excess body weight—particularly around the neck and abdomen—can increase airway resistance and reduce respiratory efficiency during sleep. Insulin resistance and metabolic dysfunction further amplify inflammatory signaling and impair neuromuscular control of the airway, increasing vulnerability to collapse (25).
Inflammation and Gut Health
Chronic low-grade inflammation contributes to tissue swelling, airway narrowing, and altered neuromuscular signaling. Disruption of gut microbial balance and increased intestinal permeability can perpetuate systemic inflammation, indirectly affecting airway stability and sleep quality (26).
Nutrient Status and Muscle Tone
Adequate levels of micronutrients such as magnesium, vitamin D, and essential trace minerals are required for normal muscle function, nerve signaling, and respiratory control. Deficiencies may impair upper airway muscle tone and worsen sleep-disordered breathing over time (27).
Hormonal Regulation
Hormones play a central role in airway muscle tone, fat distribution, and sleep architecture. Thyroid dysfunction, shifts in sex hormones, and altered cortisol rhythms have all been associated with increased sleep apnea risk and severity (28).
Environmental and Lifestyle Influences
Environmental toxin exposure, chronic stress, poor sleep hygiene, alcohol use, and sedative medications can further relax airway muscles and disrupt respiratory control during sleep, compounding existing airway instability (29).
Why Root-Cause Awareness Matters
Addressing these contributors does not replace conventional medical treatment for sleep apnea. Instead, it allows care to be personalized and supportive, targeting inflammation, metabolic dysfunction, hormonal balance, and nervous system regulation that may otherwise undermine treatment success.
This systems-based perspective provides the foundation for integrative strategies that complement conventional therapies, improve treatment tolerance, and support overall physiological stability over time.
Functional Medicine Strategies That Support Sleep Apnea Care
Functional medicine strategies are designed to support, not replace, medically indicated treatments such as CPAP, oral appliances, or surgical interventions. When used alongside conventional care, these approaches aim to improve airway physiology, reduce contributing stressors, and enhance overall treatment tolerance and long-term outcomes.
Rather than focusing on a single intervention, functional medicine addresses the internal environment that influences airway stability, neuromuscular control, inflammation, and sleep quality.
Nutrition and Metabolic Support
A nutrient-dense, anti-inflammatory dietary pattern can help reduce systemic inflammation and support healthy weight regulation—both of which directly influence airway stability during sleep. Clinical emphasis is typically placed on:
Whole, minimally processed foods
Adequate protein intake to support muscle tone and tissue repair
Healthy fats and fiber to improve metabolic signaling
Limiting ultra-processed foods, excess sugar, and late-night alcohol (30)
Improving insulin sensitivity and metabolic flexibility may reduce airway collapsibility and support more stable breathing during sleep.
Gut Health Optimization
Because gut health plays a central role in immune and inflammatory regulation, restoring microbial balance can have downstream effects on airway function and sleep quality. Supportive strategies may include:
Targeted probiotic or prebiotic support
Anti-inflammatory dietary adjustments
Temporary elimination of foods that provoke immune activation (31)
Reducing gut-driven inflammation may help decrease upper airway tissue swelling and improve neuromuscular coordination over time.
Hormone Evaluation and Regulation
Thyroid hormones, cortisol rhythms, and sex hormones all influence sleep architecture, airway muscle tone, and fat distribution. Functional evaluation may involve comprehensive thyroid testing and, when appropriate, assessment of adrenal and sex hormone patterns to guide individualized support (32).
Hormonal regulation is particularly relevant when sleep apnea coexists with fatigue, weight resistance, or disrupted circadian rhythms.
Environmental and Lifestyle Optimization
Environmental exposures and lifestyle factors can significantly influence respiratory control during sleep. Supportive interventions often focus on:
Reducing exposure to environmental toxins
Improving indoor air quality
Minimizing alcohol or sedative use
Establishing consistent sleep–wake schedules
Managing light exposure and stress physiology (33)
These changes help stabilize nervous system signaling and reduce factors that promote airway relaxation during sleep.
Movement, Exercise, and Positional Support
Regular physical activity supports metabolic health, improves sleep quality, and enhances respiratory muscle strength. For some individuals, positional therapy—such as side sleeping in cases of supine-dependent obstructive sleep apnea—may also reduce apnea severity when used alongside standard treatments (34).
Together, these strategies help create a physiological environment that supports airway stability, nervous system balance, and long-term resilience—allowing conventional sleep apnea treatments to work more effectively.
How Acupuncture Can Support Sleep Apnea Management
Within an integrative care model, acupuncture is used as a supportive modality to help regulate the nervous system, reduce inflammatory signaling, and improve physiological factors that influence breathing during sleep. It is not a standalone treatment for sleep apnea, but rather a complementary approach used alongside medically indicated airway therapies.
Nervous System Regulation and Autonomic Balance
Sleep apnea is associated with heightened sympathetic nervous system activity and reduced parasympathetic tone, particularly during sleep. Research suggests acupuncture can influence autonomic balance by modulating neural signaling pathways involved in stress regulation and respiratory control (35).
By supporting parasympathetic activity, acupuncture may help:
Reduce nighttime stress responses
Improve sleep continuity
Support more stable breathing patterns during sleep
These effects are particularly relevant for individuals with sleep apnea who experience fragmented sleep, elevated nighttime arousal, or difficulty adapting to airway therapies.
Inflammation Reduction and Sleep Quality
Chronic inflammation contributes to airway tissue swelling and neuromuscular instability, increasing vulnerability to obstruction. Evidence indicates acupuncture can influence inflammatory mediators and reduce systemic inflammatory signaling, which may indirectly support airway patency and sleep quality (36).
Clinically, patients often report:
Deeper, more restorative sleep
Fewer nighttime awakenings
Improved morning energy and recovery
While subjective improvements vary, reduced inflammatory burden may enhance overall treatment response when acupuncture is used alongside standard care.
Upper Airway Muscle Tone and Respiratory Support
Some clinical studies suggest acupuncture may influence neuromuscular signaling involved in respiration, potentially supporting upper airway muscle coordination and tone. These effects are thought to occur through central nervous system modulation rather than direct mechanical airway change (37).
When used in conjunction with conventional therapies, this neuromuscular support may contribute to improved breathing stability during sleep in selected individuals.
What the Research Suggests
Systematic reviews and clinical studies indicate that acupuncture, when used as an adjunct, may:
Improve subjective sleep quality
Support autonomic regulation
Reduce symptom burden in some individuals with sleep apnea
Reductions in apnea–hypopnea index (AHI) have been observed in some studies, though results are variable and not consistent across all populations (38).
Importantly, the most reliable benefits are seen when acupuncture is integrated with conventional sleep apnea treatment, rather than used in isolation.
Integrating Acupuncture Into a Comprehensive Sleep Apnea Plan
Managing sleep apnea effectively often requires a coordinated, multidisciplinary approach. Conventional medical therapies—such as positive airway pressure, oral appliances, or surgical interventions—play a critical role in maintaining airway safety and reducing immediate health risks. Integrative therapies are most effective when they are used to support these treatments by improving physiological regulation rather than competing with standard care.
Within a comprehensive care plan, acupuncture may be integrated to help:
Support nervous system regulation and stress resilience
Reduce inflammatory burden that can worsen airway instability
Improve sleep quality and tolerance of airway therapies
Enhance overall physiological regulation that influences breathing during sleep
When acupuncture is combined with functional medicine strategies—such as metabolic optimization, hormone regulation, gut health support, and environmental awareness—it can help address contributors that may otherwise limit the effectiveness of conventional sleep apnea treatments (39).
Importantly, integrative care is most effective when it is personalized. Factors such as sleep apnea severity, coexisting medical conditions, medication use, stress load, and overall health status all influence which supportive strategies are appropriate and how they should be timed within care.
Benefits of a Systems-Based, Integrated Approach
When conventional and integrative strategies are coordinated appropriately, individuals may be better positioned to:
Continue evidence-based airway therapy for safety
Reduce symptom burden and daytime fatigue
Improve long-term adherence to treatment
Support whole-body health beyond sleep alone
Treatment focuses on restoring balance across interconnected physiological systems rather than addressing symptoms in isolation.
→ Acupuncture & Nervous System Regulation
Taking a Whole-Person Approach to Sleep Apnea Care
Sleep apnea is best understood as a systems-driven condition, shaped by the interaction of airway structure, breathing mechanics, metabolic health, inflammation, nervous system regulation, and lifestyle influences. While maintaining airway patency during sleep is essential for safety, long-term outcomes are often improved when care extends beyond symptom control alone.
A whole-person approach recognizes that contributors such as chronic inflammation, insulin resistance, hormonal imbalance, gut dysfunction, stress physiology, and environmental exposures can all influence airway stability and sleep quality. Addressing these factors does not replace conventional treatment—but it can reduce physiological strain, improve treatment tolerance, and support more durable health outcomes.
Integrative care is most effective when it is coordinated, individualized, and grounded in evidence-based medicine. For many individuals, this means continuing appropriate medical therapy while simultaneously supporting the regulatory systems that govern breathing, recovery, and adaptation.
By viewing sleep apnea through a systems-based, integrative lens, individuals are better positioned not only to protect their health during sleep, but also to improve daytime energy, cognitive performance, metabolic balance, and long-term cardiovascular resilience (40).
Next Steps for Integrative Sleep Apnea Support
If you have been diagnosed with sleep apnea—or suspect sleep-disordered breathing may be contributing to fatigue, brain fog, metabolic challenges, or poor sleep quality—an integrative evaluation can help identify contributing factors and clarify supportive options.
You may request a free 15-minute consultation with Dr. Martina Sturm to review your health concerns and outline appropriate next steps within a root-cause, systems-based framework.
You may request a free 15-minute consultation with Dr. Martina Sturm to review your health concerns and outline appropriate next steps within a root-cause, systems-based framework.
Frequently Asked Questions About Sleep Apnea
What is sleep apnea and why is it serious?
Sleep apnea is a sleep-related breathing disorder in which airflow repeatedly pauses or becomes restricted during sleep. These events disrupt oxygen delivery and sleep quality, placing stress on the cardiovascular, metabolic, and nervous systems over time.
What are the most common symptoms of sleep apnea?
Common symptoms include loud snoring, gasping or choking during sleep, frequent awakenings, morning headaches, unrefreshing sleep, excessive daytime fatigue, difficulty concentrating, and mood changes such as irritability or low mood.
Can sleep apnea cause fatigue even if I sleep all night?
Yes. Sleep apnea fragments sleep and reduces oxygen delivery, preventing the body from reaching restorative sleep stages. As a result, individuals may feel exhausted despite spending adequate time in bed.
Why is sleep apnea considered a systemic health condition?
Sleep apnea affects more than sleep quality. Repeated oxygen fluctuations and stress activation increase the risk of high blood pressure, heart disease, insulin resistance, metabolic dysfunction, cognitive impairment, and mood disorders.
How is sleep apnea diagnosed?
Sleep apnea is typically diagnosed using an overnight sleep study, either in a sleep laboratory (polysomnography) or through validated home sleep apnea testing. Severity is commonly measured using the apnea–hypopnea index (AHI).
Is CPAP always required for sleep apnea?
CPAP is considered first-line therapy for moderate to severe obstructive sleep apnea, but treatment recommendations depend on severity, airway anatomy, and individual tolerance. Some individuals with mild sleep apnea may use oral appliances or positional strategies under medical guidance.
Can lifestyle changes improve sleep apnea?
Lifestyle factors such as weight management, side sleeping for position-dependent apnea, reducing alcohol or sedative use, regular physical activity, and consistent sleep routines can help reduce severity—often alongside medical therapy.
How does a functional medicine approach differ in sleep apnea care?
Functional medicine evaluates contributing factors such as metabolic health, inflammation, gut function, nutrient status, hormonal balance, and stress physiology. These factors are addressed to support overall physiology while standard airway treatments remain in place.
Can acupuncture help with sleep apnea?
Acupuncture may support sleep quality, nervous system regulation, inflammation reduction, and breathing stability in some individuals. It is best used as an adjunct to conventional sleep apnea treatment, not as a replacement.
Still Have Questions?
If the topics above reflect ongoing symptoms or unanswered concerns, a brief conversation can help clarify whether a root-cause approach is appropriate.
Resources
National Heart, Lung, and Blood Institute – Sleep apnea
American Academy of Sleep Medicine – Obstructive sleep apnea: overview
American Academy of Sleep Medicine – Clinical guideline for the evaluation, management, and long-term care of obstructive sleep apnea
The Lancet Respiratory Medicine – Pathophysiology of upper airway collapse in obstructive sleep apnea
Sleep – Systems biology of sleep-disordered breathing
Chest – Sleep fragmentation and intermittent hypoxia in obstructive sleep apnea
Circulation – Intermittent hypoxia, sympathetic activation, and cardiovascular stress in obstructive sleep apnea
The Lancet Diabetes & Endocrinology – Metabolic and endocrine consequences of obstructive sleep apnea
Hypertension – Hypertension and vascular dysfunction in obstructive sleep apnea
Diabetes Care – Insulin resistance and metabolic syndrome in sleep apnea
Neurology – Cognitive impairment and accident risk in sleep-disordered breathing
Endocrine Reviews – Immune and endocrine dysregulation in obstructive sleep apnea
Sleep Medicine Reviews – Long-term health outcomes of untreated sleep apnea
American Journal of Respiratory and Critical Care Medicine – Treatment selection and phenotyping in obstructive sleep apnea
The New England Journal of Medicine – Efficacy of continuous positive airway pressure therapy
Sleep Medicine – CPAP adherence and clinical outcomes
Chest – Bilevel positive airway pressure in complex sleep apnea
Journal of Clinical Sleep Medicine – Oral appliance therapy for obstructive sleep apnea
Annals of Internal Medicine – Comparative effectiveness of CPAP and mandibular advancement devices
Otolaryngology–Head and Neck Surgery – Surgical management of obstructive sleep apnea
The Laryngoscope – Hypoglossal nerve stimulation and advanced surgical options for sleep apnea
European Respiratory Journal – Obesity, airway resistance, and sleep-disordered breathing
Nature Reviews Endocrinology – Hormonal regulation of respiration and sleep-disordered breathing
Journal of Applied Physiology – Nasal breathing, nitric oxide signaling, and airway stability
Sleep Medicine Reviews – Mouth breathing, airway collapse, and sleep quality
Frontiers in Immunology – Systemic inflammation and neuromuscular dysfunction in sleep apnea
Nutrients – Micronutrients, neuromuscular control of respiration, and sleep health
Chronobiology International – Circadian rhythm regulation and sleep hygiene interventions
Sports Medicine – Exercise and positional therapy in obstructive sleep apnea
Autonomic Neuroscience – Autonomic nervous system dysregulation in sleep apnea
Frontiers in Endocrinology – Thyroid and sex hormone influences on sleep-disordered breathing
Frontiers in Nutrition – Anti-inflammatory dietary patterns and sleep quality
Neuroscience & Biobehavioral Reviews – Gut microbiota, inflammatory signaling, and sleep disorders
Brain, Behavior, and Immunity – Probiotics, gut permeability, and systemic inflammation in sleep disturbance
Sleep Medicine Reviews – Long-term outcomes of systems-based approaches to sleep apnea
Sleep Medicine Reviews – Autonomic regulation and sleep-disordered breathing
Chest – Respiratory control mechanisms in obstructive and central sleep apnea
Journal of Clinical Endocrinology & Metabolism – Hormonal influences on sleep architecture and breathing
Frontiers in Psychiatry – Integrative and multidisciplinary care models for sleep apnea
Sleep Medicine Reviews – Adjunctive and non-pharmacologic therapies in sleep apnea management