Yeast Infections Beyond the Vagina: Hidden Candida Symptoms and Root Causes
How Gut Dysbiosis, Hormones, Medications, and Immune Dysfunction Drive Chronic Candida Overgrowth—and How Functional Medicine Restores Balance
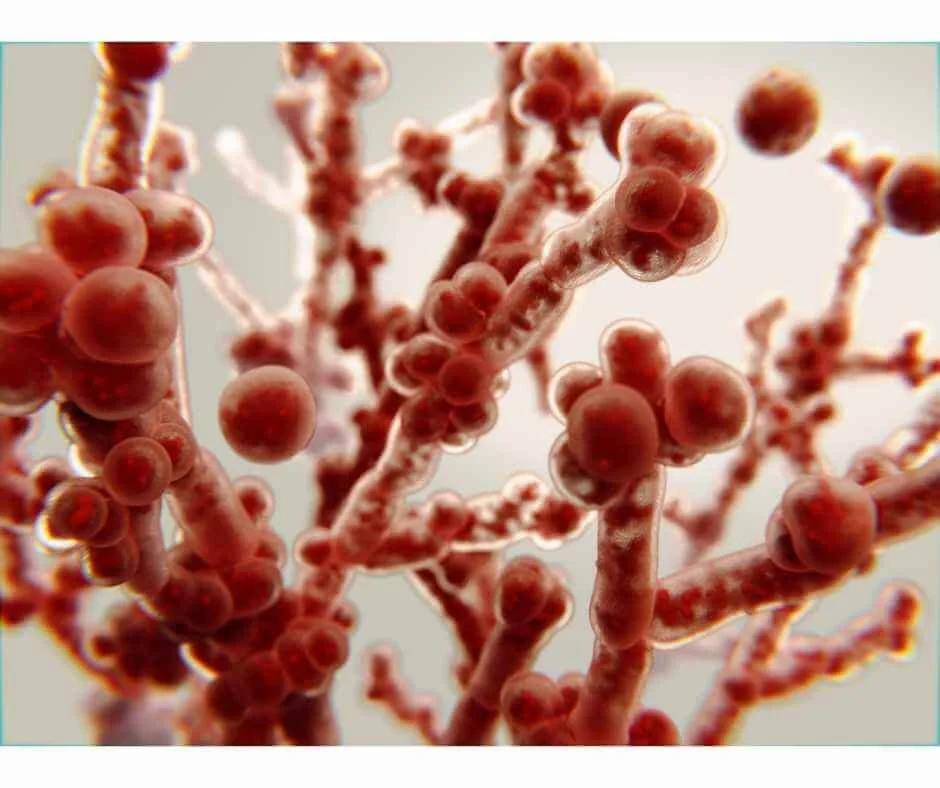
Yeast infections are commonly thought of as a vaginal issue—but this narrow view misses the much bigger picture. Candida and other yeast species can overgrow in the gut, mouth, skin, urinary tract, sinuses, and even systemically, often producing symptoms that are vague, chronic, and easily misattributed to stress, hormones, or “normal aging.” Brain fog, fatigue, digestive issues, recurrent infections, mood changes, and sugar cravings are frequently overlooked signs of yeast imbalance rather than isolated problems.
In functional medicine, yeast overgrowth is not treated as a random infection to suppress, but as a signal of deeper imbalance involving the microbiome, immune function, hormones, toxic exposures, and metabolic health. Many patients struggling with recurring yeast infections also have underlying contributors such as gut dysbiosis, mold or mycotoxin exposure, blood sugar instability, or immune suppression—factors that must be addressed for lasting resolution.
This article explores the hidden presentations of Candida overgrowth, why conventional antifungal treatments often fail to prevent recurrence, and how a root-cause, systems-based approach can help restore microbial balance. You’ll also learn when yeast infections may be a downstream sign of broader issues requiring evaluation through Advanced Functional Lab Testing or support through Detoxification & Environmental Medicine, particularly when mold exposure or chronic inflammation is involved.
For readers dealing with overlapping symptoms such as digestive dysfunction, fatigue, or recurrent infections, this discussion builds on concepts explored in
→ Mold Toxicity Symptoms, Mycotoxins in Food, and Detox Strategies
→ Gut Dysbiosis: When the Microbiome Is Out of Balance,
helping connect the dots between yeast overgrowth and whole-body health.
What Causes Yeast Infections?
There are multiple species of Candida that naturally live in the human body, but Candida albicans is the strain most commonly associated with problematic yeast infections. It can reside in the gut, mouth, skin, intestines, and other tissues without causing symptoms—until the internal balance is disrupted.
Yeast infections tend to develop when the microbiome is out of balance or when the immune system is under strain. When Candida is no longer kept in check by beneficial bacteria and immune defenses, it can begin to overgrow. In more severe cases, Candida can migrate through the gastrointestinal lining or enter the bloodstream, leading to serious and, in rare situations, life-threatening infections.
One of the most common triggers for yeast overgrowth is antibiotic use. While antibiotics can be lifesaving, they also indiscriminately eliminate beneficial bacteria that normally suppress Candida. Without that protective bacterial population, yeast is given an open opportunity to proliferate—sometimes long after the antibiotic course has ended.
Early signs of Candida overgrowth are often subtle and systemic rather than localized. These may include:
Nausea
Brain fog or difficulty concentrating
Joint or muscle pain
Headaches
White coating on the tongue
Sugar cravings
Chronic fatigue
Halitosis (bad breath)
Digestive discomfort, bloating, or irregularity
Because these symptoms overlap with many other conditions, yeast overgrowth is frequently missed or misattributed.
Beyond antibiotics, several underlying conditions and environmental factors can increase the likelihood of developing yeast infections. These include chronic stress, blood sugar imbalance, hormonal shifts, toxic exposures, and gut dysbiosis—topics explored further in From Digestion to Disease: The Alarming Effects of Dysbiosis
When yeast infections become recurrent or resistant to standard treatments, deeper evaluation through Advanced Functional Lab Testing and support via Detoxification & Environmental Medicine may be necessary to identify and address the true root cause rather than repeatedly treating symptoms alone.
Risk Factors for Yeast Infections
Yeast infections rarely happen without context. Certain hygiene habits, lifestyle factors, and underlying health conditions can increase susceptibility, while in other cases, normal physiological shifts—such as hormonal changes—are enough to tip the balance.
Vaginal Yeast Infections (Vaginal Candidiasis)
Vaginal yeast infections are among the most recognized forms of Candida overgrowth, but they are rarely caused by a single factor. Common contributors include:
Chronic stress
Diabetes or blood sugar dysregulation
Mold or mycotoxin exposure
The Standard American Diet (high in sugar and processed foods)
Pregnancy or hormonal birth control
Antibiotic use (current or past)
Heavy metal toxicity
Many of these factors directly impact immune function, hormone signaling, and the vaginal and gut microbiome. For patients experiencing recurrent vaginal yeast infections—especially those that temporarily improve but keep returning—this pattern often points to a deeper imbalance explored in Hormone & Metabolic Optimization and Detoxification & Environmental Medicine.
Oral Thrush (Mouth and Throat Yeast Infections)
Yeast infections of the mouth and throat, commonly referred to as thrush, are uncommon in healthy adults. They are more frequently seen in infants under one month of age or in individuals with compromised immune defenses.
Risk factors for thrush include:
Recent or repeated antibiotic use
Diabetes
Cancer or chemotherapy
HIV/AIDS
Use of immunosuppressive medications
Additional contributors that are often overlooked include:
Smoking
Denture use
Chronic dry mouth, which may be related to mouth breathing, medications, or nervous system dysregulation
These cases often overlap with broader microbial imbalance and may warrant evaluation through → Advanced Functional Lab Testing, particularly when symptoms persist or recur.
Invasive Candidiasis (Systemic Infection)
Invasive candidiasis occurs when Candida enters the bloodstream and spreads to organs such as the kidneys, eyes, heart, or brain. This is a serious medical condition and most often occurs in hospital or medically complex settings.
Risk factors include:
Diabetes
Kidney failure
Chemotherapy
Implanted medical devices
Recent surgery (including organ transplantation)
Prolonged or high-dose antibiotic use
While invasive candidiasis is less common, its existence highlights an important functional medicine principle: Candida becomes dangerous when terrain, immunity, and barriers are compromised.
Although yeast infections can range from mild to severe, there are effective functional medicine strategies for both prevention and treatment. Addressing root contributors—rather than repeatedly suppressing symptoms—offers the best chance for long-term resolution, especially in chronic or recurrent cases.
How to Reduce Your Risk of Yeast Infections
It’s always best to work with a qualified functional medicine practitioner to confirm whether yeast is truly the underlying issue and to develop an approach tailored to your individual physiology. Yeast infections—especially when they are recurrent—often reflect a deeper imbalance rather than an isolated problem. In some cases, they may even be a downstream sign of more complex contributors such as mold or mycotoxin exposure, gut dysbiosis, or immune dysfunction.
From a functional medicine perspective, prevention is about restoring balance rather than targeting yeast in isolation. The strategies below work best when applied together. Addressing only one factor—such as diet or supplements—rarely leads to lasting resolution, which is why a systems-based, holistic approach is key.
Diet: Supporting Microbial Balance
Diet plays a meaningful role in shaping the gut and vaginal microbiome and influencing Candida colonization.
In general, reducing foods high in sugar, refined carbohydrates, and ultra-processed ingredients is foundational. These foods disrupt microbial balance and can create an internal environment that favors yeast overgrowth. Alcohol can have a similar effect by impairing immune function and altering gut flora.
Candida overgrowth is frequently associated with digestive symptoms such as bloating, irregular stools, and IBS-like patterns. Emerging research also suggests a connection between Candida, intestinal permeability (leaky gut), and inflammatory bowel conditions, including Crohn’s disease and ulcerative colitis, when yeast penetrates the intestinal lining.
Dietary patterns that may help reduce symptoms include:
Low-FODMAP diet
Mediterranean diet
Anti-Candida (Candida cleanse) diet
Mold-aware detox diet
The Mediterranean and low-FODMAP diets are particularly helpful for reducing inflammation, which is important because inflammation weakens the gut barrier and allows yeast and other opportunistic organisms to thrive.
Anti-Candida and mold-focused diets typically involve removing foods such as:
Sugar
Refined flour
Certain dairy products
While these approaches may improve symptoms for some individuals, there is currently no evidence that diet alone can prevent candidiasis. Yeast overgrowth is multifactorial, which is why dietary changes are most effective when combined with broader gut, immune, and detoxification support.
Overall, reducing processed foods appears to lower Candida colonization. Incorporating fatty-acid–rich coconut oil, which has mild antimicrobial properties, may also be supportive for some individuals.
Fermented foods such as kimchi, sauerkraut, kefir, and kombucha can help support microbial diversity, though they should be introduced carefully in those with SIFO or significant dysbiosis.
Hygiene: Protecting the Microbiome
Everyday hygiene choices can either support or disrupt microbial balance.
Helpful strategies include:
Avoiding douching or overwashing, which can dry vaginal tissue, disrupt beneficial bacteria, and introduce endocrine-disrupting chemicals
Choosing toxin-free personal care products
Supporting oral microbiome health
Douching, in particular, has been shown to worsen vaginal microbiome imbalance and may allow infections to spread further into the reproductive tract.
Oral thrush risk is reduced when oral hygiene supports—not sterilizes—the microbiome. Commercial toothpastes and mouthwashes often eliminate both beneficial and harmful microbes. Gentler alternatives include:
Water flossing
Fluoride-free toothpaste
Natural dental floss without PFAS (“forever chemicals”)
Homemade mouth rinses using diluted essential oils, baking soda, and water
More aggressive herbal or antimicrobial oral protocols are sometimes necessary but should be personalized and guided clinically.
It’s also worth noting that corticosteroid inhalers can disrupt oral microbial balance and contribute to thrush if the mouth is not rinsed properly after use.
Clothing & Moisture Control
For vaginal yeast infections, environmental moisture matters.
Helpful practices include:
Avoiding tight or synthetic clothing
Choosing breathable fabrics
Sleeping without underwear if prone to recurrent infections
Cotton underwear is particularly supportive because it absorbs moisture and heat rather than trapping it, creating an environment less favorable for yeast growth.
Similarly, fungal infections such as athlete’s foot or toenail fungus are more likely when feet remain damp or enclosed. Allowing feet to air out at home and rotating footwear can make a meaningful difference.
Zinc and Recurrent Yeast Infections
Emerging research suggests a relationship between zinc status and Candida behavior. In a small study, a zinc-containing cream reduced reinfection rates in women with recurrent vaginal yeast infections.
While larger studies are still needed, this relationship helps explain why zinc deficiency may contribute to persistent symptoms. Candida appears to aggressively utilize zinc when levels are low, triggering inflammatory responses that contribute to burning and itching sensations.
For some individuals, targeted zinc support—topical or internal—may help keep Candida populations in check and reduce recurrence when used as part of a broader, individualized plan.
Treating Yeast Infections
Antifungal medication and antibiotics are often used to treat yeast infections. However, antifungal-resistant strains can develop just like when antibiotics are overused.
There are also adverse side effects to these types of medications such as elevated liver enzymes (a sign of liver damage), nervous system disorders, gastrointestinal issues, visual disturbances, and cardiovascular disease. Because of the associated risks, I recommend functional medicine alternatives to preventing and treating infections.
Ozone Therapy
Ozone therapy has shown promising results in both the prevention and treatment of yeast infections, particularly in cases where infections are recurrent or resistant to standard approaches. Its therapeutic effects are multifactorial and align well with the underlying mechanisms involved in Candida overgrowth.
Key benefits of ozone therapy include:
Reducing inflammation
Supporting immune modulation
Improving oxygen delivery to low-oxygen tissues
Broad antimicrobial activity against bacteria, fungi, and viruses
Vaginal or rectal ozone insufflation can be especially helpful in yeast-related conditions. Ozone exerts its antifungal effect by oxidizing components of the yeast cell wall, impairing Candida’s ability to survive and replicate. Research has demonstrated ozone’s effectiveness against a range of pathogenic microorganisms, including Candida species.
Localized ozone injections may also be useful in cases such as toenail fungus, where poor circulation and low oxygen tension allow fungal organisms to persist despite topical treatments.
As with any advanced therapy, ozone is most effective when used within a comprehensive, individualized treatment plan rather than as a standalone intervention.
Herbs and Supplements
Targeted herbal and probiotic strategies can play a supportive role in managing Candida overgrowth when chosen carefully and used appropriately.
Certain probiotic strains—particularly Bifidobacterium, Lactobacillus, and the beneficial yeast Saccharomyces boulardii—have demonstrated activity against specific Candida strains. These organisms help restore microbial balance by competing with yeast for space and resources while supporting immune signaling within the gut.
Beyond strain selection, delivery form matters. Many conventional probiotics are vulnerable to stomach acid, heat, and oxidation. Spore-based probiotics are more resilient and are better able to survive transit through the digestive tract, becoming active in the small intestine where support is often most needed.
Other compounds that may help limit Candida growth include:
Berberine
Boric acid (short-term, targeted use only)
Capric acid
Coconut oil
Oregano oil
Garlic-derived compounds
Undecylenic acid
It’s important to note that while these agents can be helpful, prolonged or unsupervised use may disrupt beneficial microbes or place unnecessary strain on detoxification pathways.
Traditional Chinese Medicine also offers both internal and topical herbal approaches for yeast-related conditions, selected based on constitutional patterns, immune status, and the presence of heat, dampness, or deficiency. These strategies are best applied within a personalized clinical framework.
What to Do if You Suspect You Have a Yeast Infection
Because yeast overgrowth can present in many different ways, testing is often necessary to confirm what’s actually driving symptoms. Depending on the presentation, stool testing, urine markers, blood work, and vaginal or oral microbiome assessments may be used to evaluate Candida activity and overall microbial balance.
If you’re experiencing symptoms commonly associated with yeast infections—especially if this is your first episode or if infections keep returning—it’s important to work with a functional medicine practitioner who can look beyond surface-level treatment. A root-cause approach helps determine why yeast is overgrowing rather than simply suppressing symptoms temporarily.
Restoring microbial balance is rarely straightforward or one-size-fits-all. Factors such as gut health, immune function, hormone balance, toxic exposures, and nutrient status all influence how the body responds to treatment. In addition, some herbal and antimicrobial strategies—while useful in the right context—can disrupt beneficial microbes if used incorrectly or for too long, which is why guidance matters.
Support is available to help you navigate testing and personalized treatment options. You can request a free consultation with Dr. Martina Sturm to explore functional strategies that address the root cause of your symptoms rather than simply managing flare-ups.
Frequently Asked Questions About Yeast Infections
Can men get yeast infections too?
Yes. Although yeast infections are more commonly discussed in women, men can also develop them. Common areas include the genitals, mouth (oral thrush), skin folds, and toenails. Symptoms may involve itching, redness, soreness, irritation, or discharge depending on the location.
What causes yeast infections?
Yeast infections most often result from an overgrowth of Candida albicans. Common triggers include antibiotic use, hormonal shifts (such as pregnancy or hormonal birth control), chronic stress, immune suppression, mold exposure, and diets high in sugar or highly processed foods.
Are yeast infections contagious?
Yeast infections are not typically classified as sexually transmitted infections. However, Candida can be transferred between partners during sexual contact. When infections are recurrent, it may be appropriate for both partners to be evaluated.
How do I know if my symptoms are from a yeast infection?
Symptoms can include itching, burning, redness, swelling, discharge, digestive issues, fatigue, brain fog, or mood changes. Because these symptoms overlap with many other conditions, testing is the only reliable way to confirm whether yeast overgrowth is present.
What role does diet play in yeast infections?
Diet can strongly influence Candida activity. Diets high in sugar and processed foods tend to promote yeast overgrowth, while anti-inflammatory dietary patterns—such as Mediterranean, low-FODMAP, or Anti-Candida approaches—support microbial balance and reduce inflammation.
How can yeast infections be prevented naturally?
Prevention focuses on reducing factors that allow yeast to thrive. Helpful strategies include wearing breathable cotton underwear, avoiding tight clothing, reducing sugar and alcohol intake, using toxin-free personal care products, avoiding douching or overwashing, and supporting gut health through diet and probiotics. Addressing deeper contributors such as stress, hormonal imbalance, or environmental exposures is often essential.
What natural treatments are available for yeast infections?
Functional and herbal approaches may include ozone therapy, spore-based probiotics, garlic-derived compounds, oregano oil, berberine, boric acid (short-term, targeted use), coconut oil, and undecylenic acid. These approaches aim to support the body’s terrain while reducing reliance on antifungal medications.
Can ozone therapy help with yeast infections?
Yes. Ozone therapy improves oxygen delivery, supports immune regulation, and has broad antimicrobial activity against Candida. Vaginal or rectal insufflation and localized ozone injections, such as those used for toenail fungus, can be effective when appropriately indicated.
When should I seek medical care?
Medical evaluation is recommended for recurrent infections, severe or persistent symptoms, or signs of systemic involvement such as fatigue, fever, or widespread skin changes. Functional testing can help identify underlying contributors such as immune dysfunction, mold exposure, or metabolic imbalance.
Why do yeast infections keep coming back?
Recurring yeast infections often point to unresolved root causes, including gut dysbiosis, mold or mycotoxin exposure, heavy metal burden, hormonal imbalance, or immune dysfunction. Long-term relief depends on identifying and addressing these contributing factors rather than repeatedly treating symptoms alone.
Resources
PMC – Candida albicans: Top 10 Herbs and Supplements to Beat It
PMC – The gut, the bad and the harmless: Candida albicans as a commensal and opportunistic pathogen in the intestine
StatPearls – Risk Factors for Candidiasis
Functional Medicine University – How to Prevent and Treat Candida Overgrowth and Avoid a Herxheimer Reaction
PMC – Candida albicans Biofilms and Human Disease
Functional Medicine Institute – A Functional Medicine Candida Overgrowth Protocol: Testing, Nutrition, and Supplements
Frontiers in Microbiology – Mycobiome in the Gut: A Multiperspective Review
PMC – Mediterranean Diet as a Tool to Combat Inflammation and Chronic Diseases: An Overview
Cleveland Clinic – What to Know About Candida Cleanse
CDC – Preventing Candidiasis
Science Translational Medicine – Zinc Prevents Vaginal Candidiasis by Inhibiting Expression of an Inflammatory Fungal Protein
PubMed – Is Zinc Deficiency Behind the Dramatic Spike in Yeast Infections?
PMC – Ozone Therapy for Dermatological Conditions: A Systematic Review
ScienceDirect – The Efficacy of Gaseous Ozone Against Different Forms of Candida albicans
PubMed – Safety and Efficacy of a Novel Vaginal Anti-infective, TOL-463, in the Treatment of Bacterial Vaginosis and Vulvovaginal Candidiasis: A Randomized, Single-Blind, Phase 2 Controlled Trial
PMC – Application of Probiotic Yeasts on Candida Species–Associated Infection
Journal of Biological Chemistry – Capric Acid Secreted by Saccharomyces boulardii Inhibits Candida albicans Filamentous Growth, Adhesion, and Biofilm Formation
PMC – Undecylenic Acid Inhibits Morphogenesis of Candida albicans