Acupuncture for PCOS: How It Supports Hormonal Regulation and Ovulation
How acupuncture influences cycle regularity, androgen balance, and stress physiology in women with PCOS
Polycystic Ovary Syndrome (PCOS) is not a single condition with a single cause. It is a heterogeneous syndrome shaped by different underlying drivers, including metabolic signaling, inflammation, stress physiology, and hormonal suppression. This variability explains why symptoms, severity, and responses to care can differ significantly from one woman to the next (1).
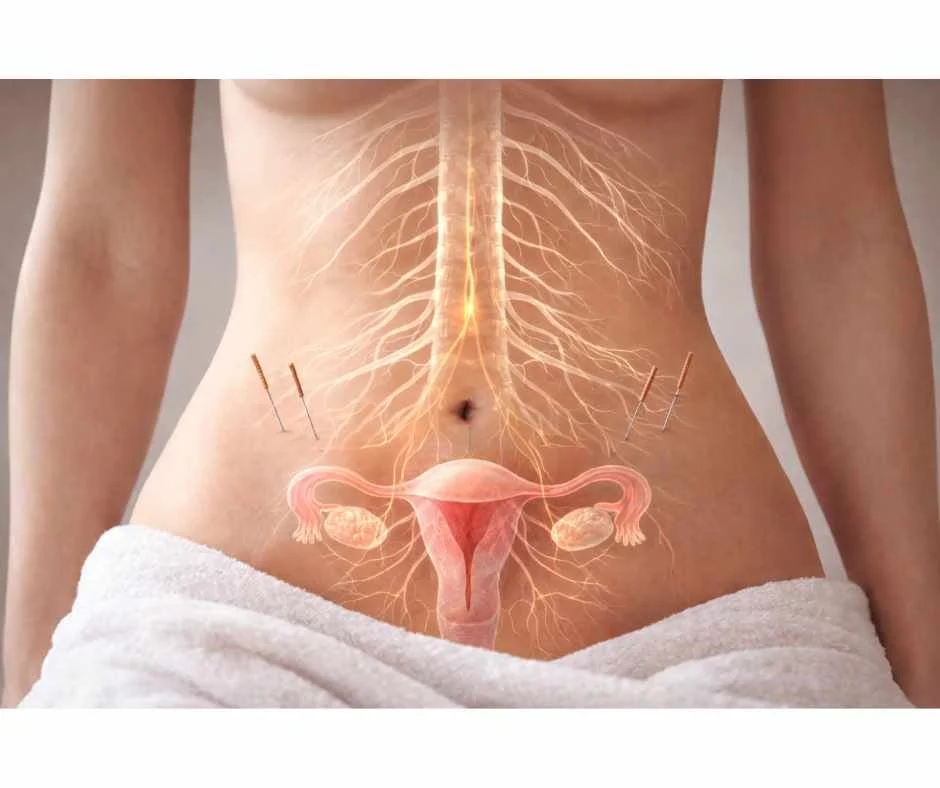
Acupuncture is commonly used as a supportive therapy in PCOS because of its ability to influence nervous system regulation, hormonal signaling, and blood flow, all of which play central roles in ovulation and menstrual cycle function (2). Rather than forcing hormonal changes, acupuncture works by supporting communication between the brain, ovaries, and other regulatory systems involved in reproductive health (3).
Research suggests that acupuncture may help support menstrual regularity, ovulatory signaling, insulin sensitivity, inflammatory balance, and stress regulation in women with PCOS (4, 5). These effects are particularly relevant given that PCOS is often characterized by disrupted signaling rather than simple hormone deficiency.
Importantly, the role acupuncture plays can vary depending on the underlying PCOS pattern. Insulin-driven, inflammatory, adrenal, and post–birth control PCOS can each respond differently to acupuncture, which is why classification and context matter when selecting supportive therapies (6).
This article explains how acupuncture supports PCOS-related hormonal signaling, ovulation, cycle regulation, and stress physiology—and when it is most effective within an integrative care plan.
How Acupuncture Affects Hormonal Signaling in PCOS
PCOS is characterized by disrupted communication between the brain, ovaries, and other regulatory systems rather than a simple deficiency or excess of a single hormone. Acupuncture is thought to influence this communication by modulating nervous system activity, neuroendocrine signaling, and local blood flow (1).
Key Regulatory Pathways Influenced by Acupuncture
Rather than acting on a single hormone, acupuncture appears to support multiple interconnected signaling systems involved in ovulation and cycle regulation:
Hypothalamic–Pituitary–Ovarian (HPO) Axis
The HPO axis coordinates ovulation and menstrual cycle timing. In PCOS, signaling along this axis is often altered, contributing to irregular cycles and impaired ovulation (2). Research suggests acupuncture may help normalize aspects of this signaling by influencing central nervous system pathways involved in hormonal feedback (3).Autonomic Nervous System Balance
Many women with PCOS exhibit increased sympathetic nervous system activity, which is associated with higher androgen production and disrupted ovulatory signaling (4). Acupuncture has been shown to promote parasympathetic activity, helping shift this imbalance and support more stable hormonal communication (5).Local Pelvic and Ovarian Circulation
In addition to central regulatory effects, acupuncture can influence local blood flow. Improved circulation to the ovaries and pelvic region has been observed in some studies, which may support ovarian responsiveness to hormonal signals involved in follicle development and ovulation (6).
A Regulatory—not Suppressive—Effect
Importantly, these effects are regulatory rather than suppressive. Acupuncture does not override the endocrine system or impose hormonal changes. Instead, it appears to support the body’s ability to regulate its own signaling pathways—an important distinction in PCOS, where dysregulation rather than loss of function is the core issue (7).
Acupuncture and Menstrual Cycle Regulation in PCOS
Irregular or absent menstrual cycles are one of the most common features of PCOS and reflect disrupted ovulatory signaling rather than a primary uterine problem (1). In many cases, cycles are irregular because communication between the brain and ovaries is inconsistent, leading to delayed or absent ovulation.
How Acupuncture May Support Cycle Regularity
Acupuncture has been studied for its potential role in supporting menstrual cycle regulation in women with PCOS by influencing central regulatory signaling rather than replacing hormones:
Neuroendocrine Coordination
Research suggests acupuncture may influence cycle patterns by modulating neuroendocrine signaling involved in follicular development and ovulation timing (2). These effects appear to occur through changes in central nervous system activity rather than direct hormonal intervention.Ovulatory Signaling vs. Forced Menstruation
Several studies have observed improvements in cycle regularity among women with PCOS receiving acupuncture, particularly when irregular cycles are driven by ovulatory dysfunction rather than structural abnormalities (3). Rather than inducing menstruation artificially, acupuncture appears to support the regulatory processes that allow cycles to occur more consistently over time.Stress Physiology and Cycle Timing
Stress signaling plays a significant role in menstrual regulation. Elevated sympathetic nervous system activity and chronic stress can interfere with ovulatory timing and luteal phase signaling (4). By promoting parasympathetic activity and reducing stress-related neuroendocrine interference, acupuncture may help remove barriers to more consistent cycle signaling (5).
Why Changes Are Often Gradual
Cycle regulation in PCOS is typically a progressive process, not an immediate shift. Improvements may be subtle at first and depend on the degree of signaling disruption present prior to treatment. This variability reflects the underlying heterogeneity of PCOS rather than inconsistency of acupuncture itself (6).
Why this structure works
It is important to note that cycle regulation is often gradual. Improvements may be subtle at first and depend on how disrupted signaling was prior to treatment. This variability reflects the underlying heterogeneity of PCOS rather than inconsistency of the therapy itself (6).
Acupuncture and Ovulation Support in PCOS
Ovulatory dysfunction is a defining feature of PCOS and is often the underlying reason for irregular cycles and fertility challenges (1). In many cases, ovulation does not occur consistently because hormonal signaling between the brain and ovaries is disrupted, rather than because the ovaries are incapable of releasing an egg.
How Acupuncture May Support Ovulatory Signaling
Acupuncture has been studied for its potential role in supporting ovulation in women with PCOS by influencing regulatory signaling pathways, not by directly stimulating egg release:
Neuroendocrine Regulation of Ovulation
Research suggests acupuncture may influence ovulatory signaling by modulating neuroendocrine pathways involved in follicle development and luteinizing hormone (LH) signaling (2). These effects appear to be regulatory rather than stimulatory, meaning acupuncture does not force ovulation but may help normalize the conditions under which ovulation can occur.Autonomic Nervous System Balance
Increased sympathetic nervous system activity has been associated with impaired ovulation and elevated androgen production in PCOS (3). Acupuncture may help reduce sympathetic overactivity, supporting a neuroendocrine environment that is more favorable for coordinated ovulatory signaling (4).Pelvic and Ovarian Blood Flow
Improved pelvic blood flow has been observed in some studies examining acupuncture in PCOS (9). Adequate circulation supports oxygen and nutrient delivery to ovarian tissue and may enhance ovarian responsiveness to hormonal cues involved in follicle maturation and ovulation.
Why Ovulatory Responses Vary
Clinical outcomes related to ovulation vary depending on the dominant PCOS pattern and the degree of signaling disruption present prior to treatment. For some individuals, ovulatory markers improve over time, while others experience more gradual changes that reflect restoration of regulatory balance rather than immediate ovulation (6).
Acupuncture, Insulin Sensitivity, and Inflammation in PCOS
Insulin resistance and chronic low-grade inflammation are common features of PCOS and can significantly influence androgen production, ovulatory signaling, and overall metabolic stability (8). Even when glucose levels appear within conventional ranges, altered insulin signaling and inflammatory stress can disrupt hormonal regulation.
How Acupuncture May Influence Metabolic and Inflammatory Signaling
Acupuncture has been studied for its potential effects on insulin sensitivity and inflammatory balance by influencing regulatory systems upstream of metabolism, rather than acting directly on glucose or hormones:
Autonomic Nervous System and Insulin Signaling
Increased sympathetic nervous system activity has been associated with insulin resistance and elevated inflammatory markers, while parasympathetic activity supports metabolic regulation (2). Acupuncture appears to influence this autonomic balance, which may indirectly support improved insulin signaling and metabolic responsiveness (3).Inflammatory Pathway Modulation
Research suggests acupuncture may affect inflammatory signaling by reducing pro-inflammatory cytokine activity and improving circulation (10). In PCOS, chronic inflammation can amplify androgen production and interfere with ovulatory signaling, so reducing inflammatory burden may help improve overall hormonal communication rather than targeting hormones directly (5).
Acupuncture as a Complementary—Not Primary—Metabolic Intervention
Importantly, restoring balance in PCOS is rarely achieved through a single intervention. When insulin resistance is a primary driver, acupuncture does not replace metabolic, nutritional, or lifestyle support. Instead, it functions as a complementary therapy by reducing stress-related interference, improving nervous system regulation, and helping create a physiological environment that is more receptive to metabolic balance and hormonal regulation (6).
Why Responses Vary
Clinical responses depend on the individual’s dominant PCOS pattern and baseline metabolic regulation. Women with insulin-driven or inflammatory PCOS may notice gradual improvements in energy, cycle stability, or symptom intensity over time—reflecting changes in systemic regulation rather than immediate metabolic correction (7).
Acupuncture and Stress Physiology in PCOS
Stress physiology plays a central role in PCOS, particularly in patterns where adrenal signaling and nervous system dysregulation contribute to androgen excess and ovulatory disruption (1). Chronic activation of the stress response can interfere with reproductive hormone signaling by altering communication between the brain, adrenal glands, and ovaries.
Many women with PCOS exhibit increased sympathetic nervous system activity, which is associated with elevated cortisol output, impaired ovulatory signaling, and increased androgen production (11). Over time, this heightened stress response can compound metabolic and inflammatory drivers, making symptoms more persistent and less responsive to isolated interventions.
Acupuncture has been shown to influence autonomic nervous system balance by reducing sympathetic activity and promoting parasympathetic tone (3). This shift supports a more regulated stress response, which may help reduce neuroendocrine interference with ovulation and menstrual cycle signaling (4).
In addition to autonomic effects, acupuncture has been associated with changes in stress-related neurochemicals, including modulation of cortisol and endogenous opioid activity (12). These changes may contribute to improvements in sleep quality, emotional regulation, and perceived stress—factors that indirectly influence hormonal balance in PCOS.
Importantly, stress physiology does not operate in isolation. Elevated stress signaling can worsen insulin resistance, increase inflammatory burden, and amplify androgen activity (6). By supporting nervous system regulation, acupuncture may help reduce this compounding effect, allowing other regulatory systems involved in PCOS to function more effectively.
Which PCOS Patterns May Benefit Most From Acupuncture
Because PCOS is driven by different underlying physiological patterns, the way acupuncture supports regulation can vary depending on the dominant driver (1). Acupuncture does not target a single hormone or symptom; instead, it influences nervous system balance, neuroendocrine signaling, circulation, and stress physiology. These effects may be more relevant in certain PCOS patterns than others.
Patterns Where Acupuncture Is Often Most Supportive
Rather than being applied uniformly, acupuncture tends to be most effective when matched to the individual’s dominant regulatory disruption:
Adrenal and Inflammatory PCOS
Acupuncture is often particularly supportive in adrenal and inflammatory PCOS, where stress physiology, immune signaling, and nervous system dysregulation play a central role (2). In these patterns, its effects on autonomic balance and inflammatory modulation may help reduce interference with ovulatory and hormonal communication.Insulin-Driven PCOS
In insulin-driven PCOS, acupuncture is best understood as a complementary therapy rather than a primary intervention. While it does not replace metabolic or nutritional strategies, its ability to reduce stress-related signaling and support nervous system regulation may help create conditions that allow metabolic interventions to be more effective over time (3).Post–Birth Control PCOS
For individuals with post–birth control PCOS, acupuncture may support the gradual restoration of ovulatory signaling by helping regulate stress responses and improve communication between the brain and ovaries following prolonged hormonal suppression (4). In these cases, acupuncture is used to support regulation rather than artificially accelerate recovery.
Because PCOS patterns can overlap and shift, the role of acupuncture is best understood within the context of the individual’s dominant physiological drivers rather than applied as a uniform solution across all cases (5).
How Traditional Chinese Medicine Views PCOS Patterns
In Traditional Chinese Medicine (TCM), PCOS is not viewed as a single diagnosis but as a pattern-based condition involving disruptions in regulatory systems related to digestion, circulation, stress response, and reproductive function (1). These patterns often overlap and evolve over time, aligning with modern understanding of PCOS as a heterogeneous syndrome rather than a uniform disease process.
A Pattern-Based, Systems-Oriented Framework
Common TCM patterns associated with PCOS may involve:
Impaired metabolic transformation
Stress-related dysregulation
Disrupted communication between central regulatory systems and the ovaries
Rather than treating symptoms in isolation, acupuncture is used to support systemic balance and coordination across these pathways. This pattern-based framework parallels contemporary models of neuroendocrine, metabolic, and autonomic regulation and helps guide individualized acupuncture treatment while remaining compatible with modern physiological interpretations of PCOS (2).
When Acupuncture Works Best as Part of a Broader Care Plan
PCOS is shaped by interacting regulatory systems rather than a single pathway. Because of this, acupuncture tends to be most effective when it is used as part of a coordinated care plan, rather than as a standalone intervention aimed at one symptom or hormone (1).
Acupuncture’s primary role is to support regulatory capacity—including nervous system balance, stress physiology, circulation, and neuroendocrine communication. When these systems are under chronic strain, even well-designed metabolic or lifestyle interventions may not produce consistent results (2). In this context, acupuncture can help reduce interference and improve system responsiveness.
This integrative role is especially relevant when multiple drivers are present. For example, metabolic stress, inflammation, and chronic sympathetic activation often coexist in PCOS, each amplifying the others over time (3). By supporting autonomic regulation and stress resilience, acupuncture may help create conditions in which other interventions can work more effectively rather than competing against ongoing physiological stress (4).
Acupuncture is most effective when it is integrated into a broader, coordinated approach to care. In PCOS—and in health more broadly—restoring balance typically involves supporting multiple regulatory systems at the same time. Acupuncture plays an important role in this process by helping the body adapt, respond, and regulate across systems, while other aspects of care address specific metabolic, inflammatory, or hormonal factors (5).
Individual response reflects differences in physiology, baseline regulation, and overall care strategy. Approaching acupuncture as part of an integrative plan supports sustainable regulation and aligns with the complex, interconnected nature of PCOS (6).
Acupuncture as Part of an Integrative Approach to PCOS Care
PCOS is shaped by interacting regulatory systems rather than a single isolated pathway, which is why acupuncture tends to be most effective when used as part of a coordinated care plan rather than a standalone intervention (1).
Acupuncture’s Role Within an Integrative Framework
Acupuncture’s primary contribution is support of regulatory capacity, including:
Nervous system balance
Stress physiology
Circulation
Neuroendocrine communication
When these systems are under chronic strain, even well-designed metabolic, nutritional, or lifestyle interventions may not produce consistent results (2). In this context, acupuncture can help reduce physiological interference and improve overall system responsiveness.
Supporting Multiple Drivers Simultaneously
This integrative role is especially relevant when multiple drivers are present. In PCOS, metabolic stress, inflammation, and chronic sympathetic activation often coexist, each amplifying the others over time (3). By supporting autonomic regulation and stress resilience, acupuncture may help create conditions in which other interventions can work more effectively rather than competing against ongoing physiological stress (4).
Why Integration Matters for Sustainable Regulation
Acupuncture is most effective when integrated into a broader, coordinated approach to care. In PCOS—and in health more broadly—restoring balance typically involves supporting multiple regulatory systems simultaneously. Acupuncture plays an important role by helping the body adapt, respond, and regulate across systems, while other aspects of care address specific metabolic, inflammatory, or hormonal factors (5).
Individual response reflects differences in physiology, baseline regulation, and overall care strategy. Approaching acupuncture as part of an integrative plan supports sustainable regulation and aligns with the complex, interconnected nature of PCOS (6).
→ Acupuncture & Nervous System Regulation
You may request a free 15-minute consultation with Dr. Martina Sturm to review your health concerns and outline appropriate next steps within a root-cause, systems-based framework.
Frequently Asked Questions About Acupuncture for PCOS
Can acupuncture help regulate menstrual cycles in PCOS?
Acupuncture may support menstrual cycle regularity in PCOS by influencing neuroendocrine signaling, autonomic nervous system balance, and stress physiology involved in ovulation timing. Rather than inducing menstruation, it appears to support the regulatory processes that allow cycles to occur more consistently over time. Response varies depending on underlying PCOS drivers and baseline cycle disruption.
Can acupuncture help with ovulation in women with PCOS?
Acupuncture may support ovulatory signaling by helping regulate communication between the brain and ovaries and by reducing stress-related interference. It does not force ovulation or stimulate egg release directly. Changes in ovulatory markers, when they occur, tend to reflect gradual improvements in regulatory balance rather than immediate effects.
How often should acupuncture be done for PCOS?
Treatment frequency is individualized and depends on symptoms, cycle patterns, and overall regulatory stability. Many people begin with more consistent sessions to support nervous system and hormonal regulation, then adjust frequency as cycle signaling and symptoms change. A licensed practitioner determines timing based on response rather than a fixed schedule.
Is acupuncture safe for people with PCOS?
Acupuncture is generally considered safe when performed by a licensed practitioner using sterile, single-use needles. Most side effects are mild and temporary, such as brief soreness or minor bruising at needle sites. Safety considerations may vary based on individual health history.
Can acupuncture help with insulin resistance or inflammation in PCOS?
Research suggests acupuncture may support insulin sensitivity and inflammatory balance indirectly by influencing autonomic nervous system activity and inflammatory signaling. It is best viewed as a supportive therapy rather than a primary metabolic intervention, particularly when insulin resistance or inflammation is a dominant driver.
Does acupuncture help with stress, anxiety, or sleep issues related to PCOS?
Acupuncture has been shown to support parasympathetic nervous system activity and reduce sympathetic overactivation, which may help regulate stress physiology, sleep quality, and emotional resilience. These effects can indirectly influence hormonal and metabolic regulation in PCOS.
Should acupuncture be combined with other approaches for PCOS?
PCOS is rarely driven by a single factor. Acupuncture is most effective when integrated into a broader care approach that addresses dominant drivers such as metabolic regulation, inflammation, stress physiology, and hormonal signaling. Combining approaches supports more stable and sustainable regulation.
Still Have Questions?
If the topics above reflect ongoing symptoms or unanswered concerns, a brief conversation can help clarify whether a root-cause approach is appropriate.
Resources
National Institutes of Health – Polycystic Ovary Syndrome (PCOS)
Human Reproduction – Effects of acupuncture on ovulation and endocrine function in women with polycystic ovary syndrome
Fertility and Sterility – Acupuncture for polycystic ovary syndrome: a randomized controlled trial
Autonomic Neuroscience – Modulation of the autonomic nervous system by acupuncture in women with PCOS
American Journal of Obstetrics and Gynecology – Acupuncture improves menstrual frequency in women with polycystic ovary syndrome
Endocrine Reviews – Autonomic nervous system activity in polycystic ovary syndrome
Diabetes Care – Effects of acupuncture on insulin resistance in patients with polycystic ovary syndrome
Journal of Clinical Endocrinology & Metabolism – Inflammatory markers and insulin resistance in polycystic ovary syndrome
Human Reproduction Update – Acupuncture and fertility outcomes in women with polycystic ovary syndrome
Brain, Behavior, and Immunity – Anti-inflammatory effects of acupuncture: mechanisms and clinical relevance
Autonomic Neuroscience – Acupuncture-mediated reduction of sympathetic nerve activity in PCOS
Psychoneuroendocrinology – Acupuncture and stress hormone regulation