Your Gut, Hormones & Medications: How Common Drugs Disrupt Digestion and Detox Pathways
PPIs, antibiotics, birth control, and NSAIDs can quietly drain key nutrients, weaken the microbiome, and inflame the gut—here’s how to protect and rebuild.
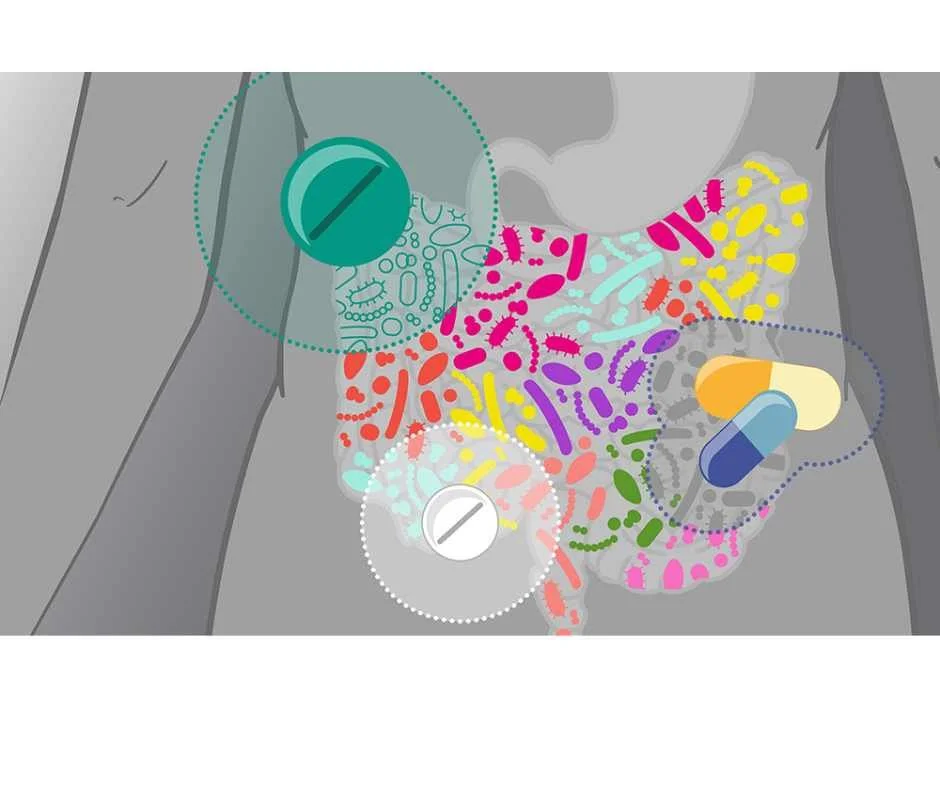
Your gut and hormones form the foundation of overall health, regulating digestion, detoxification, metabolism, immune signaling, mood, and fertility. When these systems function well, the body maintains balance and resilience. Yet millions of people take medications every day that quietly interfere with these core processes—often without immediate or obvious warning signs.
Medications such as acid blockers (PPIs), antibiotics, hormonal birth control, and NSAIDs are widely used to manage common symptoms. While they can be helpful in the short term, long-term or repeated use may compromise the gut lining, disrupt the microbiome, impair nutrient absorption, and increase strain on detoxification pathways. These effects tend to accumulate gradually and are frequently overlooked as contributors to chronic or unexplained symptoms.
The consequences are often subtle at first. Bloating, fatigue, anxiety, brain fog, acne, thyroid changes, or irregular menstrual cycles may appear intermittently and seem unrelated. In many cases, they reflect downstream effects of medications altering digestion, hormone metabolism, and immune signaling—disrupting the body’s natural healing and detox rhythms.
The Hidden Cost of Common Medications: Nutrient Depletion
Many prescription and over-the-counter medications don’t just affect symptoms—they interfere with how the body absorbs, synthesizes, and utilizes essential nutrients. This impact often goes unnoticed because deficiencies develop slowly, even in people eating what appears to be a “healthy” diet.
Over time, medication-related nutrient depletion can undermine energy production, nervous system function, hormone balance, immune resilience, and detoxification capacity. These deficiencies rarely occur in isolation; they compound one another, amplifying gut dysfunction and systemic inflammation.
Before examining specific drugs, it’s important to understand one foundational principle: when digestion is impaired, everything downstream suffers. This is especially true for medications that alter stomach acid—the first step in the digestive cascade.
1. Acid Blockers (PPIs & H2 Blockers)
PPIs such as Prilosec and Nexium, and H2 blockers like Pepcid, are commonly used to manage reflux, ulcers, and indigestion. While often effective short term, long-term acid suppression alters the digestive environment in ways that directly impair nutrient absorption and microbial balance.
Deplete: Magnesium, Zinc, Iron, Calcium, Vitamin B12, Vitamin D (1)
Why it matters
Stomach acid is not the problem—it is essential for digestion and defense. Adequate acid allows the body to break down proteins, absorb minerals and vitamins, activate digestive enzymes, and protect against pathogens.
Chronic acid suppression reduces absorption of vitamin B12, magnesium, zinc, calcium, and vitamin D, nutrients critical for nervous system health, bone integrity, immune function, and cellular energy production. (2)
Vitamin D deficiency is now recognized as a potential consequence of long-term PPI use. Low vitamin D further compromises calcium absorption, increasing osteoporosis and fracture risk.
Magnesium, required for over 300 enzymatic reactions—including cardiac and neurological regulation—becomes progressively depleted with prolonged acid suppression. (3)
Unchecked B12 deficiency can lead to anemia, cognitive changes, and irreversible neurological damage.
Health impact
Fatigue, depression, anxiety, and brain fog from low B12, zinc, and vitamin D
Osteoporosis and fractures due to impaired calcium and vitamin D absorption
Anemia from reduced iron and B12 uptake
Neuropathy, numbness, or tingling with prolonged B12 deficiency
Muscle cramps, arrhythmias, or seizures associated with low magnesium
Increased susceptibility to infections (e.g., C. difficile, pneumonia) as gastric acid–based pathogen defense declines
Stomach Acid, Digestion & Acid Blockers
Acid blockers are among the most widely prescribed medications, yet stomach acid is central to healthy digestion. It initiates protein breakdown, mineral absorption, microbial defense, and vitamin B12 assimilation via intrinsic factor.
When acid is chronically suppressed, the result is often nutrient malabsorption, microbiome disruption, vitamin D and B12 deficiency, and increased fracture risk—not resolution of the underlying problem.
Healthy stomach acid supports:
Protein digestion into amino acids
Mineral absorption (magnesium, calcium, zinc, iron)
Defense against foodborne pathogens
Vitamin B12 absorption
In many cases, reflux symptoms stem from food sensitivities, microbiome imbalance, impaired motility, or structural factors such as hiatal hernia, rather than excess acid production.
Herbal & Nutritional Support for Digestion
DGL (deglycyrrhizinated licorice): Soothes the esophagus and gastric lining
Aloe vera & slippery elm: Support mucosal repair and reduce irritation
Zinc carnosine: Clinically shown to promote gastric mucosal healing
Digestive bitters & ginger: Stimulate stomach acid and enzyme secretion
Probiotics: Help rebalance the microbiome after prolonged suppression
Nutritional & Lifestyle Approaches
Eat smaller meals and avoid eating late at night
Remove common triggers (alcohol, caffeine, fried foods, refined sugar, seed oils)
Incorporate fermented foods (sauerkraut, kefir, kimchi) to support microbial diversity
Prioritize magnesium-rich foods (pumpkin seeds, leafy greens, cacao), iron-rich foods (grass-fed beef, organ meats), and vitamin D from sunlight or fatty fish
Address posture and breathing patterns—poor diaphragmatic tone can worsen reflux
Functional Medicine Approach
Assess nutrient status (serum B12, magnesium, vitamin D, iron, zinc)
Use stool and breath testing to evaluate dysbiosis or SIBO
Taper PPIs gradually while restoring digestive function (when appropriate and safe)
Support gut repair and detoxification with glutamine, collagen, and sulforaphane
Address root causes such as food sensitivities, infections, stress, or structural contributors
While acid blockers impair nutrient absorption and digestion at the very first step, antibiotics take disruption further by directly altering the microbiome itself. What may begin as short-term infection control can evolve into long-term gut dysfunction, immune imbalance, and persistent nutrient loss.
→ Gut Health & Digestive Restoration
2. Antibiotics
Antibiotics are among the most overprescribed medications in modern healthcare, frequently used when they are unnecessary or when safer, more targeted options would suffice. While they can be lifesaving in true bacterial emergencies, routine or repeated use often comes at a significant cost to the gut microbiome, immune system, and long-term metabolic and neurological health.
Deplete: Gut flora (beneficial bacteria), Vitamin K, B Vitamins
Why it matters
Antibiotics are often essential in acute, life-threatening situations. However, they do not distinguish between pathogenic and beneficial organisms. In the process of eliminating infection, antibiotics also disrupt the gut microbiome, sometimes profoundly. (4,5)
Beneficial gut bacteria play a central role in producing B vitamins and vitamin K, a nutrient critical for normal blood clotting and vascular health. (6) When microbial diversity is reduced, nutrient synthesis, immune signaling, and intestinal barrier integrity are all affected.
Microbiome disruption following antibiotics can persist for months or even years, particularly with repeated courses or broad-spectrum agents. (7) This prolonged imbalance influences digestion, immune regulation, metabolic health, and even neurological function.
Health impact
Weakened immune resilience
Digestive distress, including bloating, diarrhea, or constipation
Nutrient malabsorption and emerging food sensitivities
Increased intestinal permeability (leaky gut), contributing to systemic inflammation and autoimmune patterns
Higher risk of overgrowth (e.g., Candida) and chronic low-grade inflammation
Increased risk of asthma, allergies, and obesity (7)
Mood changes and mental health symptoms mediated by the gut–brain axis
Gut Health & Antibiotics
While antibiotics can be lifesaving, their downstream effects on the gut are often underestimated. Loss of microbial diversity impairs nutrient synthesis, immune regulation, and mucosal defense, creating a terrain more vulnerable to chronic symptoms.
Healthy gut flora are essential for:
Nutrient synthesis (B vitamins, vitamin K)
Immune balance and pathogen resistance
Neurotransmitter production and mood regulation
Maintenance of the intestinal barrier
These patterns are commonly seen in patients with persistent digestive or immune symptoms following repeated antibiotic exposure.
Herbal & Nutritional Support
Rebuilding the gut after antibiotic exposure requires intentional, targeted support. Simply “waiting it out” often prolongs dysbiosis and increases the risk of long-term digestive, immune, and inflammatory issues.
Targeted spore-based probiotics during and after antibiotic therapy to help reseed the gut and improve resilience against recurrent dysbiosis
Saccharomyces boulardii to reduce the risk of antibiotic-associated diarrhea and limit opportunistic overgrowth
Prebiotic fibers (onion, garlic, asparagus, Jerusalem artichoke) to selectively nourish beneficial commensal bacteria
L-glutamine and zinc carnosine to strengthen and repair the gut lining and support intestinal barrier integrity
Nutrient repletion, emphasizing vitamin K–rich foods (leafy greens, natto) and a B-complex as clinically indicated
Nutritional & Lifestyle Approaches
Daily fermented foods (yogurt, kefir, kimchi, sauerkraut) following antibiotic courses
Low-sugar, anti-inflammatory meals to avoid feeding dysbiosis
Bone broth or collagen to support mucosal repair
Adequate hydration, sleep, and gentle movement to restore motility and vagal tone
Functional Medicine Approach
From a functional medicine perspective, antibiotics are rarely the first—or best—option. In the vast majority of cases, herbal and targeted antimicrobial therapies are both safer and more effective, preserving the microbiome while addressing the underlying imbalance driving infection.
Prioritize herbal antimicrobials and terrain-based interventions in most infections, reserving pharmaceutical antibiotics for true medical emergencies such as sepsis, gangrene, or confirmed MRSA
Avoid routine or precautionary antibiotic use, which often worsens immune dysfunction, promotes resistance, and drives chronic gut and inflammatory conditions
Implement microbiome-protective strategies immediately when antibiotics are unavoidable, followed by a structured 4–8 week gut restoration protocol
Use stool testing and functional assessment to evaluate microbial balance, opportunistic overgrowth, and inflammatory patterns rather than defaulting to repeated antibiotic courses
Address upstream contributors to recurrent infections, including nutrient depletion, chronic stress, sleep disruption, toxic exposures, impaired detoxification, and immune imbalanceJust as antibiotics can destabilize the gut microbiome, hormonal birth control disrupts another tightly regulated system—the gut–liver–hormone axis. Synthetic hormones used in pills and hormonal IUDs don’t simply prevent pregnancy; they also influence detoxification capacity, microbial diversity, and the body’s ability to regulate mood, energy, and fertility.
3. Hormonal Birth Control (Pills & Hormonal IUDs)
Hormonal contraceptives are often prescribed as routine solutions for cycle regulation, acne, or symptom management, yet they exert system-wide effects far beyond ovulation suppression. The synthetic hormones used in pills and hormonal IUDs alter liver detoxification, gut microbial balance, and nutrient status—often with long-term consequences that are poorly explained or anticipated.
Deplete: B-vitamins (B6, B12, folate), Magnesium, Zinc, Selenium, Vitamin C, Vitamin E
Why it matters
Synthetic hormones place a sustained burden on phase I and II liver detoxification pathways and can shift the gut microbiome in ways that impair hormone recycling and immune balance. Over time, this disruption contributes to oxidative stress, mood changes, thyroid imbalance, intestinal permeability, and impaired estrogen metabolism. (8)
Because hormone clearance relies on the gut–liver axis, even subtle digestive dysfunction can amplify these effects, allowing hormones to be improperly metabolized or recirculated.
Common symptoms
PMS or PMDD
Low libido
Anxiety or depression
Hair, skin, or nail changes
Fatigue and low stress tolerance
Recurrent infections
Thyroid symptoms
Bloating and new food sensitivities
Herbal & Nutritional Support
Supporting hormone balance after—or while using—hormonal contraceptives requires restoring nutrient sufficiency, liver detox capacity, and gut integrity, rather than simply suppressing symptoms.
Vitex (Chasteberry): Supports healthy progesterone signaling and luteal phase balance
Myo-Inositol: Improves insulin sensitivity and supports ovulatory and egg health
Maca root: Supports energy, mood stability, and libido
Milk thistle & N-acetylcysteine (NAC): Strengthen phase I and II liver detoxification of synthetic hormones
Antioxidants (vitamin C, vitamin E, selenium): Buffer oxidative stress and protect cell membranes
Calcium-D-glucarate & DIM: Support estrogen metabolism and clearance
Digestive bitters: Promote bile flow and natural hormone detox through the liver and gut
Nutritional & Lifestyle Approaches
Daily cruciferous vegetables (broccoli, kale, Brussels sprouts) to support estrogen metabolism
Zinc-rich foods (pumpkin seeds, oysters) and selenium-rich foods (Brazil nuts) for thyroid and immune balance
Magnesium-rich foods (cacao, leafy greens) to support sleep, stress resilience, and nervous system regulation
Remove added sugars and industrial seed oils to reduce inflammation and insulin resistance
Prioritize vitamin C from citrus, berries, and leafy greens to support adrenal and immune health
Support the gut with probiotics and adequate fiber, recognizing that estrogen detox depends on healthy gut transit and microbial balance
Functional Medicine Approach
Assess nutrient status, including B12, folate, zinc, selenium, vitamin D, and magnesium
Use DUTCH hormone testing to evaluate estrogen, progesterone, cortisol, and hormone metabolites
Address gut permeability and dysbiosis that impair hormone clearance
Support estrogen detoxification before, during, and after discontinuing hormonal contraceptives
Develop a fertility-supportive plan when pregnancy is a goal, emphasizing nutrient repletion and cycle restoration
Guide patients through a safe, supported transition off hormonal birth control, restoring ovulation and hormonal resilience naturally
While hormonal birth control disrupts gut and hormone balance through chronic synthetic hormone exposure, NSAIDs such as ibuprofen and naproxen damage the body in a different way. These widely used pain relievers can quietly erode the gut lining, block nutrient absorption, and drive chronic inflammation—even as they temporarily suppress pain.
4. NSAIDs (Ibuprofen, Naproxen, Aspirin)
Non-steroidal anti-inflammatory drugs (NSAIDs) are widely used for headaches, musculoskeletal pain, joint inflammation, and fever. Because many are available over the counter, they are often perceived as low risk. From a gut and detox perspective, however, regular or repeated NSAID use carries meaningful downstream consequences that are frequently overlooked.
Deplete / Disrupt: Folate, Vitamin C, Iron, Potassium; gut flora and mucosal integrity
Why it matters
NSAIDs work by inhibiting cyclooxygenase (COX) enzymes and reducing prostaglandin production. While this dampens pain and inflammation signaling, prostaglandins also play essential roles in protecting the gastrointestinal lining, maintaining blood flow, supporting kidney function, and facilitating tissue repair.
When prostaglandin activity is repeatedly suppressed, the gut lining becomes more vulnerable to injury. Over time, this can impair nutrient absorption, weaken barrier integrity, and promote intestinal permeability—placing additional strain on immune regulation and detoxification pathways.
Health impact
Gastrointestinal irritation, including heartburn, bloating, ulcers, and abdominal discomfort
Increased risk of leaky gut syndrome and food sensitivities
Fatigue, anemia, and poor wound healing related to iron and folate depletion
Increased joint or tendon vulnerability associated with vitamin C depletion and impaired collagen synthesis
Kidney stress and electrolyte imbalances with long-term or high-dose use
Higher cardiovascular risk with chronic exposure
Contribution to antimicrobial resistance, compounding microbiome disruption
Herbal & Nutritional Support
Chronic pain and inflammation are rarely isolated problems. In many cases, they reflect underlying gut dysfunction, nutrient depletion, or immune imbalance that NSAIDs temporarily mask. Supporting inflammatory regulation without compromising gut integrity is key.
Curcumin (turmeric root): Modulates COX-2 activity and oxidative stress without damaging the gut lining
Ginger: Supports inflammatory balance while improving circulation and digestive comfort
Boswellia serrata: Inhibits 5-LOX pathways involved in chronic joint and connective tissue inflammation
CBD (cannabidiol): Supports endocannabinoid regulation of pain, inflammation, and mood
White willow bark: A botanical salicylate with aspirin-like effects; use cautiously and with guidance
Omega-3 fatty acids: Reduce inflammatory cytokine signaling while supporting cardiovascular and neurological health
Vitamin C and collagen: Support connective tissue repair, cartilage integrity, and gut barrier health
(Detailed pain-management protocols are explored more fully in the pain relief medications blog.)
Nutritional & Lifestyle Approaches
NSAIDs often suppress symptoms without addressing the drivers of inflammation. Rebuilding what these medications erode requires a systems-based approach.
Anti-inflammatory nutrition: Emphasize colorful vegetables, wild-caught fish, olive oil, turmeric, and berries; avoid refined sugars, processed foods, and industrial seed oils
Hydration and electrolytes: Support kidney function and cellular balance, especially with prior NSAID exposure
Movement therapy: Gentle, consistent movement improves circulation, lymphatic flow, and tissue resilience
Mind–body regulation: Stress amplifies inflammation; breathwork, acupuncture, and nervous system regulation support healing
Functional Medicine Approach
A functional medicine approach focuses on removing drivers of inflammation while restoring gut integrity and nutrient status, rather than suppressing pain signals alone.
Investigate root contributors, including food sensitivities, gut permeability, hidden infections, and nutrient deficiencies
Rebuild the gut barrier using targeted support such as L-glutamine, zinc carnosine, collagen, and probiotics
Reduce oxidative stress and detox burden with mitochondrial and liver support (e.g., NAC, alpha-lipoic acid, sulforaphane)
Safely taper NSAIDs with professional guidance while transitioning to gut-protective, anti-inflammatory strategies
Integrate care approaches that address inflammation at its source rather than perpetuating medication dependence
While NSAIDs primarily compromise health through gut injury, prostaglandin suppression, and nutrient depletion, they are only one part of a broader pain-medication landscape. Other commonly used pain relievers—such as acetaminophen, steroids, and opioids—create harm through distinct mechanisms, including oxidative stress, immune suppression, and impaired detoxification.
→ When Pain Relief Backfires: The Hidden Risks of Tylenol, NSAIDs, Steroids & Opioids
What You Can Do Now: A Gut & Hormone Recovery Plan
Medications such as PPIs, antibiotics, hormonal contraceptives, and NSAIDs may suppress symptoms, but they rarely resolve underlying dysfunction. Over time, their effects on nutrient status, the microbiome, and detoxification pathways can compound—creating new or worsening health issues. A functional and integrative approach focuses on rebuilding foundational systems so the body can regulate and heal more effectively.
1) Assess & Map
Review medication history and symptom patterns with a trained clinician
Test key markers, including micronutrients, vitamin D, B-vitamins, iron, and stool markers (microbial diversity, inflammation)
2) Rebuild the Microbiome
Use probiotics and prebiotics strategically and with proper timing
Incorporate daily fermented foods while reducing excess sugar and alcohol
3) Replete What’s Missing
PPIs / H2 blockers → B12, magnesium, zinc, iron, vitamin D
Antibiotics → targeted probiotics, vitamin K–rich foods, B-complex
Hormonal birth control → B-vitamins, magnesium, zinc, selenium, vitamins C & E
NSAIDs → folate, iron, vitamin C, potassium (as clinically indicated)
4) Heal & Protect the Gut Lining
L-glutamine, zinc carnosine, DGL, aloe
Collagen or bone broth to support mucosal repair and barrier integrity
5) Personalize the Plan
Address the why: food sensitivities, SIBO, chronic stress, low stomach acid, impaired detox capacity
Consider a clinician-guided medication taper when appropriate, with protective strategies in place
Ready to Restore Your Gut & Hormone Health?
If reflux, bloating, fatigue, mood changes, PMS/PMDD, or persistent “mystery” symptoms began after starting—or increasing—medications, a functional and integrative approach can help identify medication-related nutrient gaps, repair the gut–liver axis, and restore resilient digestion and hormone physiology.
This work often includes targeted testing, individualized nutrition, microbiome support, and careful medication review—focused on long-term regulation rather than short-term suppression.
→ Advanced Functional Lab Testing
Take the Next Step
Your free 15-minute consultation with Dr. Martina Sturm is a brief introductory call to review your concerns, explain our clinical process, and outline appropriate next steps.
Frequently Asked Questions About Medications, Gut Health, and Nutrient Depletion
Do common medications really affect gut health and nutrient levels?
Yes. Many widely used medications—including PPIs, antibiotics, hormonal birth control, NSAIDs, acetaminophen, and corticosteroids—can interfere with nutrient absorption, microbiome balance, stomach acid production, hormone metabolism, and gut lining integrity. Over time, this disruption may contribute to fatigue, food sensitivities, hormonal symptoms, digestive changes, inflammation, and chronic illness.
How do I know if my symptoms are related to medications I’m taking?
Medication-related imbalances often develop gradually and may appear unrelated at first. Common signs include new or worsening food sensitivities, fatigue or low energy, bloating or reflux, constipation, low mood or anxiety, brain fog, changes in menstrual cycles or libido, frequent infections, and poor recovery from stress or exercise.
Targeted testing—such as micronutrient panels, gut markers, and hormone assessments—can help clarify whether medications are contributing to symptoms.
Can NSAIDs, PPIs, or birth control damage the gut lining?
Yes. Several medication classes—especially NSAIDs, antibiotics, and hormonal birth control—can weaken the mucosal barrier, alter microbiome populations, and increase intestinal permeability (often referred to as “leaky gut”). This can promote inflammation, immune dysregulation, and difficulty digesting certain foods.
If antacids reduce stomach acid, how does that affect nutrient absorption?
Stomach acid is essential for breaking down proteins, sterilizing pathogens, and absorbing key nutrients such as magnesium, zinc, iron, calcium, and vitamin B12. Long-term use of acid-blocking medications can impair absorption, increasing the risk of deficiencies that affect mood, immunity, bone health, and metabolism.
Can I safely stop medications like PPIs or NSAIDs on my own?
It depends on the medication and your health history. Some drugs—including PPIs, SSRIs, and hormonal birth control—can trigger rebound symptoms or hormonal shifts if stopped abruptly. A structured, clinician-guided taper with appropriate nutritional and gut support is often the safest approach.
Are there natural alternatives for chronic pain, reflux, or hormonal symptoms?
In many cases, yes. Root-cause strategies may include optimizing diet and hydration, supporting healthy stomach acid and bile flow, using anti-inflammatory botanicals (such as turmeric, ginger, and boswellia), hormone-supportive herbs (such as vitex or maca), microbiome-rebuilding strategies (probiotics, glutamine, zinc carnosine), and lifestyle approaches like breathwork, acupuncture, movement therapy, and stress modulation.
These approaches aim to restore function rather than suppress symptoms.
How long does it take to restore nutrient and gut balance after stopping a medication?
Timelines vary. Some people notice improvements within 4–12 weeks once nutrient repletion and gut support are implemented. More complete microbiome recovery—particularly after antibiotics or long-term NSAID or PPI use—may take 6–12 months, depending on baseline health, diet, stress, and lifestyle factors.
Should I supplement if I’m taking medications that cause nutrient loss?
Often, yes. Strategic supplementation can help prevent or correct deficiencies while root causes are addressed. Needs vary by medication class:
PPIs / H2 blockers: B12, magnesium, zinc, iron, calcium, vitamin D
Antibiotics: Probiotics, vitamin K, B vitamins
Hormonal birth control: Folate, B6, B12, zinc, magnesium, selenium, vitamins C and E
NSAIDs: Folate, iron, vitamin C, potassium, and support for collagen synthesis
Supplementation should be individualized and periodically reassessed.
Can gut healing reverse medication-related symptoms?
Often, yes. When nutrient deficiencies are corrected and the gut lining and microbiome are restored, symptoms such as fatigue, hormonal imbalance, digestive distress, chronic pain, and immune reactivity frequently improve—and in some cases resolve.
When should I seek help from a functional medicine practitioner?
Professional support may be helpful if you rely on medications long term, have persistent gut symptoms despite treatment, experience unexplained fatigue, mood changes, or hormonal imbalance, want guidance tapering medications safely, or prefer a root-cause approach rather than ongoing symptom suppression.
Resources
PMC- Proton pump inhibitors and risk of vitamin and mineral deficiency: evidence and clinical implications
PubMed- The possible risks of proton pump inhibitors
FDA- FDA Drug Safety Communication: Low magnesium levels can be associated with long-term use of Proton Pump Inhibitor drugs (PPIs)
PMC- Effects of Antibiotics upon the Gut Microbiome: A Review of the Literature
PubMed- Antibiotics as Major Disruptors of Gut Microbiota
PubMed- Association of Broad-Spectrum Antibiotic Therapy and Vitamin E Supplementation with Vitamin K Deficiency-Induced Coagulopathy: A Case Report and Narrative Review of the Literature
PMC- Current understanding of antibiotic-associated dysbiosis and approaches for its management
PubMed- Oral contraceptives and changes in nutritional requirements
PMC- The dangers of NSAIDs: look both ways
PMC- Cardiovascular and gastrointestinal effects of COX-2 inhibitors and NSAIDs: achieving a balance
PMC- Kidney damage from nonsteroidal anti‐inflammatory drugs—Myth or truth? Review of selected literature
PMC- Rofecoxib caused excess heart disease
PubMed- Multiple NSAID-Induced Hits Injure the Small Intestine: Underlying Mechanisms and Novel Strategies
PMC- Challenges in tendon–bone healing: emphasizing inflammatory modulation mechanisms and treatment
PMC- NSAID therapy effects on healing of bone, tendon, and the enthesis
PMC- Intestinal permeability and inflammation in patients on NSAIDs
PMC- The structural basis for NSAID inhibition of human dihydrofolate reductase
PMC- Evidence of Drug–Nutrient Interactions with Chronic Use of Commonly Prescribed Medications: An Update
PubMed- The effect of commonly used non-antibiotic medications on antimicrobial resistance development in Escherichia coli