Ketosis: Benefits, Risks, Cortisol Effects, and When a Keto Diet Works Best
How Ketosis, Fasting, and Metabolic Flexibility Influence Blood Sugar, Thyroid Function, and Mitochondrial Health
Ketosis works—until it doesn’t. Some people experience steady energy, clear thinking, improved blood sugar, and a sense that their metabolism is finally working with them. Others feel depleted, anxious, wired, or stuck—even while following a keto diet precisely.
These different outcomes aren’t random, and they’re not a reflection of willpower or discipline. They reflect how ketosis shifts cellular energy production, stress signaling, hormone balance, and nutrient demands in the body. When those shifts are supportive, ketosis can be a powerful therapeutic tool. When they’re mismatched to the individual, the same approach can elevate cortisol, disrupt thyroid signaling, and stall metabolic progress.
Knowing when ketosis helps—and when it creates strain—requires moving beyond diet rules and into metabolic physiology. From this perspective, ketosis isn’t a lifestyle or a rigid prescription; it’s a metabolic strategy that can be applied with precision, cycled intelligently, and adapted to the body’s changing needs over time.
In this article, we examine what ketosis is, how it affects cortisol, thyroid function, blood sugar, and metabolic flexibility, why the “keto flu” happens, when ketogenic diets can backfire, and how to use ketosis strategically for long-term metabolic resilience.
What Is Ketosis and How Does It Work?
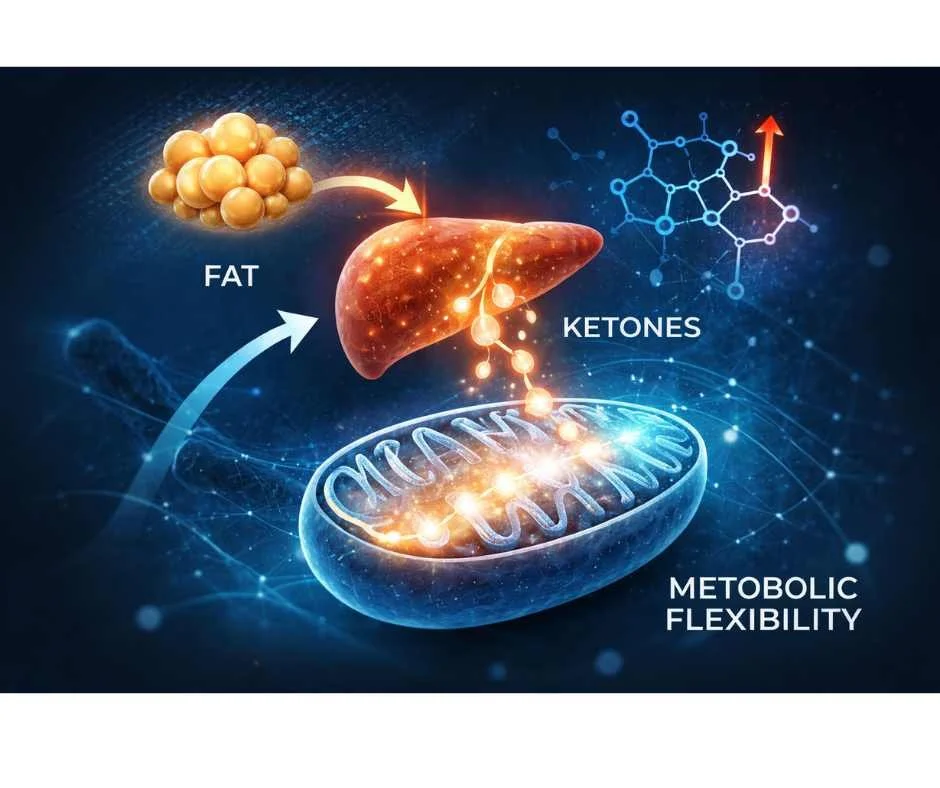
Ketosis is a natural metabolic state in which the body shifts from relying on glucose (sugar) as its primary fuel to burning fat for energy. When carbohydrate intake drops—whether through fasting or a keto diet—the liver converts fatty acids into ketone bodies, primarily beta-hydroxybutyrate (BHB), acetoacetate, and acetone. These ketones then supply energy to the brain, muscles, and other tissues. (1)
This metabolic shift is not extreme or unnatural. It evolved as a survival adaptation that allowed humans to maintain cognitive and physical function during periods of fasting or food scarcity. Today, ketosis is used intentionally to support metabolic health, insulin sensitivity, brain function, inflammation regulation, and longevity pathways. (2)
Ketosis works best when it is part of a structured metabolic strategy rather than a rigid, indefinite restriction of carbohydrates. In clinical application, ketogenic or cyclical low-carbohydrate approaches are most effective when hormone balance, thyroid function, stress physiology, and metabolic flexibility are evaluated together.
Ketosis is not simply about lowering carbohydrates—it is about how the body adapts to shifting fuel sources. When guided by physiology and monitored with objective data, it can support resilience and energy production. When applied without context, it can create unnecessary strain.
Ketosis, Fasting, and Metabolic Flexibility: Why Fuel Switching Matters
Fasting naturally induces ketosis by lowering glycogen stores and insulin levels, signaling the body to shift from glucose toward fat-derived fuel. As glycogen declines, the liver increases ketone production, allowing energy demands to be met without relying on dietary carbohydrates.
This transition can feel steady and stabilizing—or draining and disruptive. The difference typically reflects timing, stress load, sleep quality, thyroid function, and overall hormone balance—not fasting itself.
→ Weight Loss & Metabolic Health
When fasting is paired strategically with a nutrient-dense ketogenic diet, it can strengthen metabolic flexibility—the ability to switch efficiently between fat and glucose depending on activity level, stress demand, and energy availability.
Metabolic flexibility—not permanent ketosis—is what supports sustained energy, improved insulin sensitivity, and long-term metabolic resilience. The goal is not constant carbohydrate restriction, but the ability to move between fuel sources without triggering excessive cortisol, fatigue, or metabolic slowdown.
Benefits of Fasting and Ketosis for Metabolic and Cellular Health
When applied strategically, fasting and ketosis influence multiple core systems involved in energy production, metabolic regulation, and cellular repair. These effects extend beyond calorie restriction alone. Shifting from glucose to fat-derived fuel alters key signaling pathways that regulate inflammation, insulin sensitivity, mitochondrial efficiency, and longevity.
Autophagy and Cellular Renewal During Fasting
Periods of fasting activate autophagy, the body’s intrinsic cellular recycling process. During autophagy, damaged proteins and dysfunctional cellular components are broken down and cleared away, allowing healthier regeneration. This mechanism plays a central role in longevity, immune resilience, and tissue repair, and helps explain why fasting is associated with improved markers of cellular aging. (4)
How Ketosis Improves Mitochondrial Function
Ketosis supports mitochondrial function by providing a more efficient fuel source than glucose. Ketones generate ATP with reduced oxidative stress, allowing cells to produce energy more cleanly and reliably. Over time, this can enhance cellular resilience, reduce fatigue, and improve the body’s ability to meet metabolic demand—particularly in states of insulin resistance or chronic inflammation. (5)
Ketosis and Insulin Sensitivity: Blood Sugar Regulation
Fasting and ketogenic states lower circulating insulin levels, allowing insulin receptors to regain sensitivity. This stabilizes blood sugar regulation and improves metabolic signaling. Rather than forcing glucose down artificially, ketosis helps restore physiologic fuel balance and reduces the metabolic strain associated with persistent hyperinsulinemia. (6)
Hormonal Effects of Fasting and Ketosis
Fasting and ketosis influence key hormones involved in repair and energy regulation. Growth hormone secretion rises during fasting, supporting fat metabolism and tissue recovery. In appropriate metabolic contexts, androgen signaling may also improve as insulin resistance and inflammation decline. These hormonal effects remain dependent on adequate caloric intake, micronutrient status, and stress balance. (7)
Ketones and Brain Health: Cognitive and Neuroprotective Effects
Ketones provide a stable, efficient fuel source for neurons and increase levels of brain-derived neurotrophic factor (BDNF), a critical regulator of neuroplasticity and cognitive resilience. This helps explain why ketogenic strategies are studied in epilepsy, neurodegenerative disease, and cognitive decline, and why many report improved focus and mental clarity during well-supported ketosis. (8)
Benefits of Ketosis for Energy, Brain Function, and Metabolic Health
When ketosis is well tolerated and appropriately timed, it can offer benefits that extend beyond short-term weight loss. These effects arise from how ketones influence cellular energy production, inflammation, insulin signaling, and stress response—not from carbohydrate restriction alone.
Mental Clarity and Cognitive Stability
Ketones provide a steady, efficient fuel source for the brain, often supporting clearer thinking and more consistent focus. Unlike glucose, which can fluctuate with meals, sleep, and stress, ketones deliver stable energy that helps reduce the mental highs and crashes commonly experienced with high-carbohydrate patterns. (11)
Sustained Energy Without Blood Sugar Swings
By reducing rapid glucose cycling, ketosis can smooth out energy fluctuations throughout the day. Once fat adaptation is established, many notice fewer crashes between meals and more sustained physical and mental stamina. Energy becomes less dependent on constant carbohydrate intake and more reliant on stored fuel reserves.
Blood Sugar Control and Insulin Sensitivity
Ketosis lowers circulating glucose and reduces overall insulin demand, which can improve fasting glucose, A1c, and markers of insulin resistance. (12) When applied strategically, this shift supports more stable metabolic signaling and may reduce long-term risk associated with chronic hyperinsulinemia.
Anti-Inflammatory Signaling and Longevity Pathways
Ketones function not only as fuel but also as signaling molecules. They influence pathways involved in cellular repair and stress resistance, including AMPK and Nrf2. Activation of these pathways is associated with reduced oxidative stress, improved detoxification capacity, and mechanisms linked to healthy aging. (13)
Neurological Protection and Brain Resilience
The ketogenic diet has long been used therapeutically in epilepsy and continues to be studied in neurodegenerative conditions such as Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis. By supplying an alternative fuel source and reducing neuroinflammatory signaling, ketosis may help support brain resilience in metabolically vulnerable states. (14)
Potential Risks of Fasting and Ketosis: Cortisol, Thyroid, and Hormonal Balance
Fasting and ketosis can be powerful metabolic tools—but they are not universally supportive in every context. When applied too aggressively, layered on top of high stress, or continued without reassessment, they can shift from therapeutic to depleting.
Cortisol and the Stress Response
Prolonged fasting or significant calorie restriction can activate the body’s stress response, increasing cortisol output. Cortisol isn’t inherently harmful—it helps maintain blood sugar and energy during fasting—but when it remains elevated, it can suppress thyroid conversion (T4 to T3), slow metabolic rate, and contribute to fatigue, cold intolerance, disrupted sleep, or stalled weight loss. (9)
In this state, ketosis may still be present, but the body is operating from stress chemistry rather than metabolic ease.
Hormonal Sensitivity and Cyclical Fasting
Women, in particular, often respond better to cyclical fasting patterns that align with hormonal rhythms rather than daily or prolonged restriction. Estrogen, progesterone, insulin, and cortisol are tightly linked to energy availability. During periods of high stress, perimenopause, intense training, or inadequate recovery, rigid fasting can amplify imbalance rather than restore it.
→ Hormone & Metabolic Optimization
Strategic cycling—rather than constant restriction—tends to preserve hormonal stability and long-term sustainability.
Under-Eating and Deep, Prolonged Ketosis
Long-term deep ketosis combined with chronic under-eating can increase the risk of nutrient insufficiency, low energy availability, mood shifts, and hormonal disruption if not carefully monitored. (10)
When carbohydrate restriction is layered on top of poor sleep, high training load, or ongoing stress, the body may shift into conservation mode. Instead of building resilience, metabolism slows and progress plateaus.
The Real Objective: Metabolic Flexibility
The goal isn’t indefinite ketosis. It’s metabolic flexibility—the ability to move smoothly between fat and carbohydrate metabolism based on energy demands, stress load, season, and activity.
When flexibility is prioritized, fasting and ketosis can be restorative. When rigidity takes over, the same strategies can work against the body instead of supporting it.
Keto Flu Symptoms and Causes: Why It Happens and What It Means
During the first days or weeks of starting a ketogenic diet, many experience what’s commonly called the “keto flu.” (15) For some, it presents as mild fatigue or mental fog. For others, it can feel intense enough to question whether ketosis is sustainable.
Common Keto Flu Symptoms
Fatigue or low energy
Brain fog, irritability, or mood swings
Headaches or dizziness
Muscle cramps or heart palpitations
Nausea or disrupted sleep
These symptoms are not random. They reflect a temporary metabolic transition.
As the body shifts from glucose dependence to fat and ketone utilization, insulin levels fall. Lower insulin signals the kidneys to excrete more sodium, potassium, and magnesium. This rapid mineral loss—combined with reduced glycogen stores—can lead to dehydration, electrolyte imbalance, and reduced energy availability.
Without adequate mineral and caloric support, the body can feel sluggish, foggy, or depleted during this adjustment phase.
Why Keto Flu Happens
The “keto flu” is not a required or healthy part of fat adaptation. In most cases, it signals that the transition is happening too abruptly or without sufficient support.
Common triggers include:
Rapid carbohydrate restriction without gradual adaptation
Electrolyte depletion from increased urination
Inadequate dietary fat intake to fuel mitochondria
Stacking fasting with aggressive carb restriction
Overtraining, poor sleep, or chronic stress that elevates cortisol
Because cortisol and thyroid signaling strongly influence metabolic adaptation, keto flu symptoms often overlap with broader stress patterns.
When carbohydrate restriction is layered on top of high stress, intense training, or inadequate recovery, the body may struggle to adapt smoothly—regardless of how “disciplined” the diet appears.
What Keto Flu Really Means
In most cases, keto flu reflects mineral depletion, stress signaling, or insufficient fuel—not a failure of willpower.
With gradual transition, adequate electrolytes, sufficient calories, and stress support, many can enter ketosis without significant discomfort. When symptoms persist, it often indicates that the approach needs modification rather than intensification.
MCT Oil and Coconut Oil for Keto Adaptation: How They Ease the Transition
Medium-chain triglycerides (MCTs)—found in coconut oil and concentrated in MCT oil—are unique fats that can make the transition into ketosis smoother and more sustainable, especially when early fatigue or “keto flu” symptoms appear.
Why MCTs Are Metabolically Different
Unlike long-chain fatty acids, which require bile acids, pancreatic enzymes, and the L-carnitine shuttle to enter the mitochondria for oxidation, MCTs largely bypass this transport system.
That distinction becomes especially important during early ketosis. When fat adaptation is incomplete, mitochondria are often inefficient at transporting long-chain fats across the mitochondrial membrane. This bottleneck—the carnitine shuttle—can contribute to sluggishness, low energy, and difficulty producing sufficient ketones from stored fat. (16)
MCTs bypass this constraint. They are absorbed directly into the portal circulation, delivered to the liver, and rapidly converted into ketone bodies—providing quick fuel for both the brain and muscles. (17)
How MCT Oil Helps Reduce Keto Flu Symptoms
Because MCTs are converted into ketones quickly, they can provide a more immediate energy source during the adaptation phase.
Potential benefits during keto transition include:
Faster ketone production
More stable mental clarity
Reduced fatigue during carb withdrawal
Improved mitochondrial fuel availability
Smoother shift from glucose to fat metabolism
Many notice improved focus and steadier energy shortly after introducing MCT oil—even before full fat adaptation develops.
Coconut Oil vs. MCT Oil
Virgin coconut oil contains natural MCTs, primarily caprylic (C8) and capric (C10) fatty acids, though in lower concentrations than purified MCT oil. For those sensitive to concentrated MCT oil, coconut oil often provides a gentler starting point while still supporting ketone production.
Clinical Tip for Dosing
Start slowly—about 1 teaspoon once or twice daily—and increase gradually to 1–2 tablespoons as tolerated. Introducing too much too quickly may cause gastrointestinal discomfort, including loose stools or nausea.
Functional Perspective
MCTs can act like “training wheels” for mitochondria. By bypassing the carnitine shuttle, they help bridge the gap between glucose dependence and efficient fat adaptation—reducing metabolic friction during the transition into ketosis.
How to Prevent or Reduce Keto Flu Symptoms
For most, keto flu discomfort isn’t a sign that ketosis is wrong—it’s a signal that the transition needs more support. The goal is not to force fat adaptation, but to create the conditions that allow it to happen smoothly and sustainably.
How to Transition Into Ketosis Without Triggering Keto Flu
Rather than cutting carbohydrates abruptly, reduce intake gradually over 2–3 weeks while increasing clean fats such as avocado, olive oil, coconut, and MCT oil. This gives digestive enzymes, mitochondria, and hormone signaling pathways time to adjust, lowering stress on the system and improving fat adaptation.
Electrolytes and Mineral Support for Keto Flu Prevention
As insulin levels fall, the kidneys excrete more sodium and trace minerals. Without replenishment, this mineral loss can lead to headaches, fatigue, dizziness, and muscle cramps. Replacing sodium, magnesium, and potassium—through mineral salt or structured mineral support such as Quinton Isotonic or Hypertonic—helps stabilize fluid balance and reduce common keto flu symptoms.
Hydration Strategies to Reduce Keto Flu Symptoms
Increased urination is common during early ketosis. Aim for 3–4 liters of mineralized, filtered water daily to prevent dehydration, which can intensify fatigue, brain fog, and lightheadedness. Hydration alone can dramatically improve early adaptation symptoms when paired with adequate electrolytes.
Eating Enough Fat and Calories During Keto Adaptation
Avoid going low-carbohydrate and low-fat at the same time. During keto adaptation, mitochondria require sufficient fuel to learn how to oxidize fat efficiently. Chronic under-eating can slow metabolic transition, elevate stress hormones, and worsen fatigue rather than accelerate results.
Supporting Thyroid and Adrenal Function on a Keto Diet
Sleep quality, circadian rhythm alignment, stress regulation, and adequate caloric intake all influence how well the body adapts to ketosis. When cortisol is already elevated from life stress, aggressive carbohydrate restriction can push metabolism into conservation mode instead of productive fat burning.
Why Keto Flu Is a Signal—Not a Failure
Keto flu typically reflects mineral depletion, stress signaling, or insufficient fuel—not a lack of discipline. When hydration, electrolytes, calories, and recovery are addressed, many can enter ketosis without significant discomfort. If symptoms persist, the strategy often needs refinement rather than intensification.
How to Measure Ketosis: Why Ketone Testing Matters
Tracking ketone levels can provide clarity—not because there is a single “perfect number,” but because it reveals how your body responds to diet, fasting, stress, sleep, and training load. Two people can follow the same keto diet and produce very different ketone levels. Testing removes guesswork and helps distinguish true adaptation from hidden strain.
Not everyone enters or maintains ketosis at the same threshold. Stress load, sleep quality, exercise intensity, and carbohydrate timing all influence ketone production—sometimes more than food choices alone.
Urine Ketone Strips
Urine strips are inexpensive and easy to use, making them common during early keto adaptation. They measure acetoacetate, one of the three ketone bodies. However, as fat adaptation improves, urinary ketones often decline—even when ketosis is present—making this method less reliable over time.
Breath Ketone Meters
Breath meters estimate ketone production by measuring acetone. They are non-invasive and convenient but tend to be more variable and less precise, particularly when tracking small changes or long-term trends.
Blood Ketone Testing (Gold Standard)
Blood testing measures beta-hydroxybutyrate (BHB), the primary circulating ketone used by the brain and muscles. It provides the most accurate and clinically meaningful assessment of metabolic state and depth of ketosis.
When objective data is needed—especially in therapeutic or performance-focused contexts—blood ketone testing is often paired with glucose and broader metabolic markers to understand how ketosis fits into the larger physiologic picture.
→ Advanced Functional Lab Testing
Keto-Mojo: A Practical Tool for Home Monitoring
At Denver Sports & Holistic Medicine, we often recommend Keto-Mojo as a practical option for people who want reliable, at-home tracking of both ketones and glucose without unnecessary complexity.
Why Keto-Mojo Is Useful
Dual Measurement
Tracks both blood glucose and BHB, allowing calculation of the Glucose Ketone Index (GKI), which can offer insight into metabolic efficiency and fuel utilization.
Clinical Accuracy
FDA-approved and validated in research, making it suitable for clinical and personal use.
Simple Data Tracking
Syncs with the Keto-Mojo app and integrates with platforms like Apple Health or Cronometer, making it easier to observe patterns over time rather than focusing on isolated readings.
Functional Versatility
Useful for people exploring fasting, metabolic health, longevity strategies, or therapeutic ketosis under supervision.
Cost-Effective for Long-Term Use
Test strips are generally more affordable than many alternatives, which matters for ongoing tracking.
Target Ketone Ranges
Nutritional ketosis: ~0.5–3.0 mmol/L BHB
Therapeutic ketosis: ~3–5 mmol/L BHB, used selectively and under clinical supervision
These ranges are guides, not goals. Higher numbers are not inherently better, and context—symptoms, energy, hormones, and stress response—always matters more than the number alone.
Why the Keto Diet Can Raise Blood Sugar: Cortisol, Gluconeogenesis, and Stress Physiology
For many, a keto diet improves blood sugar stability and energy. For others, it can do the opposite—raising fasting glucose, increasing anxiety, or creating a “wired but tired” feeling.
When this happens, it’s rarely about carbohydrates alone. It’s often about cortisol and stress signaling.
How Low Carbohydrate Intake Activates the Stress Response
When carbohydrate intake drops very low, especially abruptly, the body may interpret this as an energy shortage. In response, the hypothalamic-pituitary-adrenal (HPA) axis activates, increasing cortisol—and to a lesser extent, adrenaline (epinephrine).
These hormones are protective. They help maintain blood sugar during fasting or perceived scarcity. Cortisol supports this by:
Stimulating gluconeogenesis (new glucose production in the liver from amino acids, glycerol, and lactate)
Increasing lipolysis (fat breakdown)
Reducing glucose uptake in muscle to preserve glucose for the brain
Even with minimal carbohydrate intake, elevated cortisol can raise fasting blood sugar by signaling the liver to produce more glucose.
Gluconeogenesis: Necessary but Sometimes Excessive
In nutritional ketosis, a moderate level of gluconeogenesis is normal and essential. The body still requires glucose for specific tissues, and the liver is designed to supply it.
Problems arise when cortisol remains chronically elevated due to stress, excessive fasting, under-eating, or sleep disruption. In that context, gluconeogenesis can become excessive rather than adaptive.
This may lead to:
Persistently elevated fasting glucose (often 90–110 mg/dL or higher)
Reduced ketone production despite strict carbohydrate restriction
Fatigue, anxiety, irritability, or unexpected sugar cravings—even while technically in ketosis
This explains why some see paradoxically higher morning glucose readings on keto despite careful adherence. (18)
How Chronic Cortisol Can Block Fat Adaptation
Sustained cortisol signaling interferes with mitochondrial efficiency and metabolic flexibility.
When the stress response dominates:
The body prioritizes glucose as emergency fuel
Insulin sensitivity can decline
Muscle protein may be broken down to sustain glucose production
Thyroid conversion (T4 → T3) may slow, reducing metabolic rate
In this state, the body shifts from repair and adaptation into fight-or-flight physiology. Fat burning becomes inefficient—not because ketosis failed, but because stress chemistry is overriding fuel flexibility. (19,20)
Common Triggers That Elevate Cortisol on Keto
Several factors can amplify this response:
Overtraining in deep ketosis
Chronic under-eating of calories or protein
Sleep deprivation or circadian rhythm disruption
Extended fasting without strategic refeeds
Pre-existing HPA axis dysregulation
Over time, these patterns can drive morning blood sugar spikes and even insulin resistance—the opposite of what most are seeking with a ketogenic approach.
How to Lower Blood Sugar on Keto: Functional Medicine Strategies
When a keto diet begins to raise blood sugar or feel depleting, the answer is rarely further restriction. More often, it involves restoring metabolic balance so the body no longer interprets carbohydrate reduction as a stress threat.
From a functional medicine perspective, the goal is to calm cortisol signaling and restore metabolic flexibility—not intensify discipline.
Strategic Carbohydrate Refeeds to Lower Cortisol on Keto
Introducing one to two structured carbohydrate-containing meals per week—such as root vegetables, fruit, or squash—can help replenish glycogen stores and support leptin and thyroid signaling. In many cases, strategic refeeds lower cortisol output and improve sleep, mood, and metabolic responsiveness.
Rather than reversing progress, controlled carbohydrate cycling often enhances long-term adaptation.
How Sleep Impacts Cortisol and Blood Sugar on a Keto Diet
Sleep is one of the strongest regulators of cortisol. Even short-term sleep deprivation can elevate cortisol by 30–40%, which may raise fasting glucose despite strict carbohydrate restriction.
Improving sleep quality through circadian rhythm alignment, evening light reduction, breathwork, acupuncture, or targeted adaptogens (such as ashwagandha, rhodiola, or holy basil) can significantly improve metabolic response to ketosis.
Electrolytes, Adrenal Support, and Blood Sugar Stability on Keto
Low insulin states increase mineral loss. Sodium, magnesium, and potassium are essential for stabilizing blood sugar and supporting adrenal signaling.
Inadequate mineral intake can amplify fatigue, lightheadedness, and stress-related glucose elevations. Mineral-rich sea salt, trace minerals, or structured mineral support may improve adaptation and reduce cortisol-driven glucose spikes.
Using Glucose and Ketone Testing to Identify Stress Patterns
Blood ketone testing, fasting glucose measurements, or continuous glucose monitors (CGMs) can reveal patterns that symptoms alone may miss.
Elevated morning glucose—often linked to the normal cortisol-driven “dawn phenomenon”—may reflect stress physiology rather than dietary failure. Tracking trends over time allows strategic adjustments instead of reactive restriction.
When a Cyclical or Mediterranean-Style Keto Approach Works Better
In the presence of thyroid imbalance, HPA axis dysregulation, high chronic stress, or intense training demands, strict continuous ketosis may not be optimal.
A cyclical ketogenic strategy or a lower-carbohydrate Mediterranean-style pattern often provides better hormonal stability, improved energy, and more sustainable metabolic flexibility.
Key Clinical Insight
“If your blood sugar rises on keto, it’s not always the food—it’s often the stress chemistry.”
The solution is not greater restriction. It is restoring metabolic balance, supporting stress physiology, and selecting an approach that works with the body rather than against it.ng metabolic balance, supporting stress physiology, and selecting a strategy that works with the body rather than against it.
Keto and Cancer: A Metabolic Support Strategy
One of the more compelling therapeutic applications of ketosis is in the context of cancer metabolism. Rather than viewing cancer solely as a genetic condition, a growing body of research recognizes that altered glucose metabolism, mitochondrial dysfunction, and insulin signaling influence how cancer cells grow and adapt.
A comprehensive exploration of the metabolic theory of cancer—including glucose dependence, insulin signaling, and mitochondrial dysfunction—is covered separately.
→ How Metabolic Health Shapes Cancer Prevention and Treatment
The Metabolic Rationale
Healthy cells are metabolically flexible—they can shift between glucose and fat depending on availability and demand. Many cancer cells, however, rely heavily on aerobic glycolysis (the Warburg effect), meaning they depend disproportionately on glucose for energy production.
By lowering circulating glucose and insulin levels, ketosis may create a metabolic environment that is less favorable for certain cancer cell pathways while continuing to supply healthy cells with ketones for efficient ATP production. (21,22,23)
Observed Benefits in Clinical Context
When used as part of a comprehensive, medically supervised plan, therapeutic ketosis has been associated with:
Improved metabolic stability and blood sugar control
Lower insulin and growth signaling such as IGF-1. (24)
Enhanced mitochondrial resilience in healthy tissue. (25)
Improved tolerance to conventional therapies in some cases. (26)
Stabilized energy and reduced treatment-related fatigue for certain patients
There are documented cases and emerging research showing meaningful clinical improvement when ketogenic strategies are applied thoughtfully. Outcomes vary, but the potential is significant when matched to the right context.
Clinical Considerations
Therapeutic ketosis in oncology is not one-size-fits-all. Patients experiencing significant weight loss, adrenal strain, thyroid imbalance, or advanced cachexia may require modified or cyclical approaches rather than deep, continuous ketosis.
The strength of this strategy lies in personalization.
Key Perspective
For some patients, ketogenic therapy has played a meaningful role in metabolic stabilization and recovery support. When guided appropriately, ketosis can be a powerful adjunct within an integrative oncology framework—helping shift the body’s terrain toward resilience while conventional treatments address the disease directly.
Metabolic Cycling and the Animal-Based Perspective
Dr. Paul Saladino, who previously promoted strict carnivore approaches, has more recently emphasized metabolic cycling—alternating between fat- and carbohydrate-based metabolism to support thyroid function, hormone balance, and long-term resilience.
This evolution reflects a broader principle within functional medicine: ketosis is most powerful when used strategically rather than indefinitely.
“Ketosis is a tool, not a prison. Flexibility is health.”
Seasonal or strategic inclusion of whole-food carbohydrates—such as fruit or honey—may help replenish glycogen, support circadian rhythm alignment, and maintain thyroid signaling in certain contexts. (18)
The larger takeaway is not about one dietary ideology over another. It is about metabolic flexibility—the ability to move between fuel sources without triggering stress chemistry or hormonal disruption.
Who May Benefit from a Keto Diet or Fasting?
Ketosis and fasting can be powerful metabolic tools when matched to the right physiology and goals.
Situations Where Ketosis or Fasting May Be Supportive
Ketogenic or fasting strategies may be appropriate in contexts such as:
Insulin resistance, prediabetes, or type 2 diabetes
Neurological conditions or age-related cognitive decline
Chronic inflammation or mitochondrial dysfunction
Weight loss efforts with underlying metabolic dysregulation
Longevity-focused metabolic protocols
In these settings, shifting fuel utilization away from constant glucose dependence may improve metabolic stability and cellular signaling.
When Greater Caution Is Needed
More individualized guidance is important in the presence of:
Adrenal dysfunction or HPA axis dysregulation
Thyroid disorders, particularly low T3 states
Low body weight or high athletic energy demands
Pregnancy or breastfeeding
In these circumstances, aggressive carbohydrate restriction or prolonged fasting may increase physiologic stress rather than improve resilience.
Ketosis is not inherently beneficial or harmful—it is context dependent. The key is matching strategy to metabolic capacity, hormone balance, and life demands.
Functional Medicine Approach to Ketosis, Fasting, and Metabolic Flexibility
Ketosis, fasting, and ketone monitoring are most effective when used as part of a precision metabolic strategy—aligned with hormone balance, stress physiology, and overall metabolic capacity.
At Denver Sports & Holistic Medicine, these tools are applied thoughtfully rather than rigidly. Lab markers such as glucose, insulin, thyroid function, cortisol patterns, and mitochondrial indicators help determine when ketosis is supportive—and when adjustment is needed.
The goal is not extreme restriction. It is fat adaptation, metabolic flexibility, and sustained energy without triggering stress physiology or hormonal disruption.
What We Monitor to Reduce Keto Side Effects and Burnout
Ketosis and fasting can be powerful metabolic therapies when personalized and cycled strategically. They may enhance mental clarity, energy stability, and long-term metabolic resilience—when matched appropriately to the individual.
Use ketosis to heal — and metabolic flexibility to thrive.
Personalized Ketosis and Fasting Based on Your Metabolism
Ketosis and fasting can be powerful metabolic tools—but only when they work with your physiology rather than against it. Hormone balance, stress load, sleep quality, thyroid function, and training demands all influence how your body responds to carbohydrate restriction.
No single keto diet or fasting protocol works the same for everyone. The key is matching strategy to metabolic capacity and adjusting when signals shift.
→ Functional & Integrative Medicine
If ketosis has improved your energy and focus, the next step is ensuring it remains sustainable. If it has left you feeling depleted, anxious, or stalled, it may require recalibration rather than abandonment.
You may request a free 15-minute consultation with Dr. Martina Sturm to review your health concerns and outline appropriate next steps within a root-cause, systems-based framework.
Frequently Asked Questions About Ketosis and Fasting
What is ketosis and how does it work?
Ketosis is a metabolic state in which the body shifts from burning glucose to burning fat for fuel. When carbohydrate intake drops, the liver produces ketone bodies—primarily beta-hydroxybutyrate (BHB)—which supply energy to the brain and muscles. This shift lowers insulin levels and changes how cells generate ATP.
How long does it take to get into ketosis?
Most people enter nutritional ketosis within 2–7 days of significantly reducing carbohydrate intake. The timeline depends on glycogen stores, metabolic health, activity level, stress load, and previous dietary patterns. Full fat adaptation can take several weeks.
What are common keto flu symptoms?
Common symptoms include fatigue, brain fog, headaches, dizziness, muscle cramps, irritability, and sleep disruption. These symptoms are typically related to electrolyte loss, dehydration, abrupt carbohydrate restriction, or elevated stress hormones during early adaptation.
How can I prevent or reduce keto flu?
Gradually lowering carbohydrates, increasing dietary fat, replenishing sodium, magnesium, and potassium, staying well hydrated, and avoiding aggressive fasting during the first weeks can significantly reduce keto flu symptoms.
Why does blood sugar sometimes rise on a keto diet?
Blood sugar may rise due to elevated cortisol rather than carbohydrate intake. Stress hormones stimulate gluconeogenesis, causing the liver to produce glucose even when dietary carbohydrates are low. Sleep deprivation, under-eating, overtraining, and prolonged fasting can contribute to this response.
Can ketosis affect thyroid function?
In some cases, prolonged calorie restriction or chronic stress during ketosis may reduce thyroid hormone conversion (T4 to T3). Adequate caloric intake, stress regulation, and cyclical carbohydrate inclusion may help support thyroid balance.
Is ketosis safe for women?
Ketosis can be safe when applied strategically. However, prolonged fasting, aggressive restriction, or high stress levels may disrupt hormonal rhythms. Many women respond better to cyclical or targeted ketogenic approaches rather than continuous deep ketosis.
What is the ideal ketone level for nutritional ketosis?
Nutritional ketosis typically ranges from 0.5–3.0 mmol/L of beta-hydroxybutyrate (BHB). Higher levels are not inherently better, and context—including energy, hormones, and stress response—matters more than the number alone.
How long should you stay in ketosis?
Ketosis does not need to be permanent. Short to moderate cycles (2–12 weeks) are commonly used to improve metabolic health. Long-term continuous ketosis may not be optimal for everyone, particularly during periods of high stress or intense training.
Who should avoid or modify a keto diet?
Caution is advised in pregnancy, breastfeeding, low body weight, thyroid disorders, adrenal dysfunction, or high athletic energy demands. Individualized guidance is important when underlying hormonal or metabolic imbalances are present.
Still Have Questions?
If the topics above reflect ongoing symptoms or unanswered concerns, a brief conversation can help clarify whether a root-cause approach is appropriate.
Resources
International Journal of Molecular Sciences – The Effects of Ketone Bodies in Pathological Conditions: Ketosis, Ketogenic Diet, Redox States, Insulin Resistance, and Mitochondrial Metabolism
Nutrition & Metabolism – The Effect of a Low-Carbohydrate, Ketogenic Diet Versus a Low-Glycemic Index Diet on Glycemic Control in Type 2 Diabetes Mellitus
Annual Review of Nutrition – Fasting, Circadian Rhythms, and Time-Restricted Feeding in Healthy Lifespan
Nutrients – The Impact of Diet Upon Mitochondrial Physiology (Review)
Nutrients – The Effects of Ketogenic Diet on Insulin Sensitivity and Weight Loss: Which Came First, the Chicken or the Egg?
The Journal of Sexual Medicine – Ketogenic State Improves Testosterone Serum Levels: Results from a Systematic Review and Meta-Analysis
Neurotherapeutics – The Ketogenic Diet as a Treatment Paradigm for Diverse Neurological Disorders
Frontiers in Endocrinology – The Influence of Extended Fasting on Thyroid Hormone: Local and Differentiated Regulatory Mechanisms
Nutrients – Effects of Very Low-Calorie Ketogenic Diet on the Hypothalamic–Pituitary–Adrenal Axis and Renin–Angiotensin–Aldosterone System
Cell Metabolism – Ketone Bodies as Signaling Metabolites
Current Nutrition Reports – Beyond Weight Loss: A Review of the Therapeutic Uses of Very-Low-Carbohydrate (Ketogenic) Diets
Aging Research Reviews – Key Signaling Pathways in Aging and Potential Interventions for Healthy Aging
Frontiers in Neuroscience – The Therapeutic Role of Ketogenic Diet in Neurological Disorders
The American Journal of Clinical Nutrition – The Ketogenic Diet: Evidence for Optimism but High-Quality Research Needed
Journal of the American College of Nutrition – Medium-Chain Triglycerides: An Update
Progress in Lipid Research – Short- and Medium-Chain Fatty Acids in Energy Metabolism: The Cellular Perspective
The Journal of Nutrition – Medium-Chain Triglycerides Are Advantageous in Promoting Weight Loss Although Not Beneficial to Exercise Performance
Pediatric Research – New Insights into the Utilization of Medium-Chain Triglycerides by the Neonate: Observations from a Piglet Model
The New England Journal of Medicine – Fuel Metabolism in Starvation
Endocrine Reviews – Stress Hormones: Physiological Stress and Regulation of Metabolism
Sports Medicine – Hormonal Exercise Response Model (HERM): A Conceptual Framework of Endocrine Reactivity to the Physical Stress of Exercise
Oncogene – Cancer as a Metabolic Disease: Implications for Novel Therapeutics
Cancer & Metabolism – Targeting Insulin Inhibition as a Metabolic Therapy in Advanced Cancer: A Pilot Safety Study
Frontiers in Nutrition – Beneficial Effects of Ketogenic Diets for Cancer Patients: A Realist Review with Focus on Evidence and Confirmation
Nutrients – Effect of Ketogenic Diets on Insulin-Like Growth Factor (IGF-1) in Humans: A Systematic Review and Meta-Analysis
Redox Biology – Ketogenic Diet Decreases Oxidative Stress and Improves Mitochondrial Respiratory Complex Activity
Nutrition & Metabolism – Ketogenic Diets as an Adjuvant Cancer Therapy: History and Potential Mechanisms
Podcast / Interview – Why Paul Saladino, MD Quit a 100% Carnivore Diet: Impacts of Cholesterol and the Value of Insulin