Intermittent Fasting for Women: How to Align Fasting With the Menstrual Cycle Without Disrupting Hormones
Cycle-Synced Fasting Strategies to Support Cortisol Balance, Progesterone Stability, and Metabolic Flexibility
Fasting is often promoted as a universal strategy for weight loss, metabolic health, and longevity—but intermittent fasting for women is far more nuanced than it is for men.
While fasting can improve insulin sensitivity, mitochondrial function, and metabolic flexibility, women’s bodies respond differently to energy restriction because of the dynamic interplay between reproductive hormones, stress signaling, and thyroid regulation. Estrogen, progesterone, cortisol, and thyroid hormones shift across the menstrual cycle—and all are sensitive to changes in food timing and perceived energy availability.
When fasting is applied without regard to the menstrual cycle, it can backfire—leading to disrupted ovulation, elevated cortisol, stalled metabolism, fatigue, mood changes, or worsening hormone symptoms. This is not a failure of discipline. It is a biological stress response.
Women are biologically wired to assess energy availability before prioritizing ovulation and long-term hormone stability. When fasting is excessive, mistimed, or layered onto chronic stress, the body may interpret it as scarcity rather than therapy—shifting into conservation mode instead of repair.
Intermittent fasting for women works best when aligned with the menstrual cycle. The follicular phase typically tolerates longer fasting windows, while the luteal phase requires shorter fasts and greater caloric support to prevent progesterone suppression and cortisol elevation.
This guide is designed for women who want to use fasting strategically—not aggressively.
Rather than offering generic fasting templates, this article explains:
How to align fasting with the menstrual cycle
When 16:8, 24-hour, or longer fasts are appropriate
How fasting shifts during perimenopause and menopause
When fasting supports hormone balance—and when it increases stress
For a broader discussion of fasting safety, metabolic readiness, and longevity physiology, those concepts are addressed separately. This article centers on practical application—how intermittent fasting can be aligned with the menstrual cycle to support metabolic health, progesterone stability, and cortisol balance without compromising hormonal resilience.
Why Intermittent Fasting Affects Women’s Hormones Differently
Intermittent fasting activates powerful metabolic pathways, including fat oxidation, autophagy, mitochondrial renewal, and improved insulin sensitivity. When appropriately applied, these processes enhance metabolic flexibility and cellular resilience.
However, intermittent fasting for women also directly influences endocrine systems that regulate:
Fertility and ovulation
Thyroid function and metabolic rate
Mood, cognition, and stress resilience
Energy availability and recovery
Estrogen, progesterone, cortisol, and thyroid hormones are highly responsive to changes in energy intake and perceived stress. Unlike men—whose reproductive physiology is less tightly coupled to energy availability—women’s hormone production is strongly linked to metabolic sufficiency.
When fasting is mistimed within the menstrual cycle, excessively prolonged, or layered onto chronic stress, the body may interpret it as food scarcity rather than a therapeutic intervention. Cortisol may rise, thyroid conversion can downshift, and ovulatory signaling may be disrupted as the body prioritizes survival over reproduction.
From an evolutionary standpoint, this response is protective. The female body is designed to confirm adequate energy availability before supporting ovulation, pregnancy, and long-term hormonal stability. When fasting is too long, too frequent, or poorly aligned with the luteal phase, it can suppress progesterone production and elevate stress signaling instead of enhancing metabolic health.
This explains why fasting protocols that work well for men—or appear effective in theory—can backfire for women when applied indiscriminately.
For women navigating fertility concerns, cycle irregularity, thyroid dysfunction, PCOS, or stress-related hormone imbalance, fasting should be integrated within a broader reproductive and metabolic framework rather than used as a standalone strategy.
→ Women’s Hormone & Reproductive Health
If fasting has previously resulted in fatigue, anxiety, disrupted sleep, missed periods, or stalled progress, this often indicates that metabolic readiness, stress load, or cycle timing requires reassessment before intensifying restriction.
Aligning fasting with the menstrual cycle allows women to access the metabolic and cellular benefits of fasting while minimizing cortisol elevation and protecting progesterone stability. (1,2)
How the Menstrual Cycle Affects Intermittent Fasting in Women
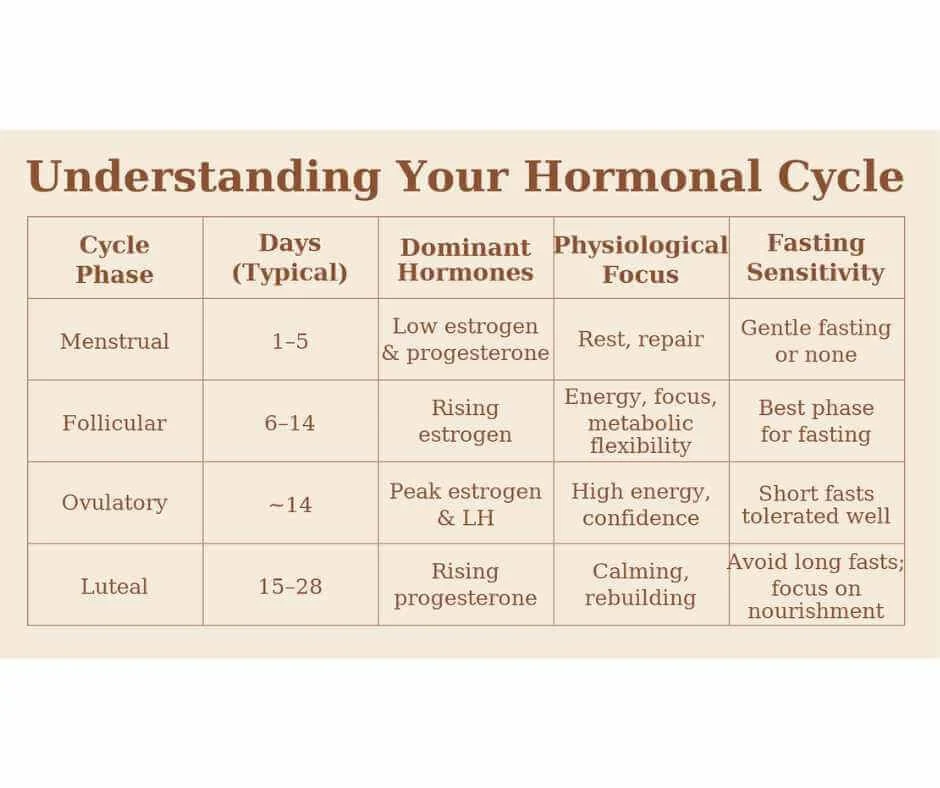
Intermittent fasting tolerance shifts across the menstrual cycle because estrogen, progesterone, insulin sensitivity, and cortisol dynamics are not constant throughout the month.
During the follicular phase, rising estrogen enhances insulin sensitivity, mitochondrial efficiency, and metabolic flexibility. This creates a physiologic environment that generally tolerates short-term energy restriction more effectively.
In contrast, the luteal phase is progesterone-dominant. Caloric needs increase, stress tolerance decreases, and insulin sensitivity is modestly reduced. Aggressive fasting during this phase may elevate cortisol and suppress progesterone production. This relationship between cortisol and fasting in women is especially important during hormonally sensitive phases of the menstrual cycle, when stress signaling can override reproductive function.
Ovulation represents a hormonally sensitive window, where excessive metabolic stress can interfere with reproductive signaling. This is why fasting and ovulation must be considered together rather than as separate variables in women’s metabolic health strategies.
Because reproductive hormones are tightly linked to perceived energy availability, fasting applied uniformly across all phases may disrupt ovulation, thyroid signaling, and sleep regulation.
Understanding this hormonal rhythm is the foundation for cycle-synced fasting strategies. (1,2)
Best Intermittent Fasting Schedule for Each Phase of the Menstrual Cycle
Intermittent fasting for women is most effective when fasting windows are synchronized with hormonal shifts across the menstrual cycle. Because estrogen, progesterone, and cortisol fluctuate throughout the month, fasting tolerance and metabolic flexibility change as well.
Below is a practical, phase-by-phase framework outlining when longer fasts are typically better tolerated—and when shorter fasting windows protect hormone stability.
Menstrual Phase (Days 1–5): Minimize Stress and Rebuild
Hormonal environment: Estrogen and progesterone are low. Energy may dip, iron needs increase, and stress tolerance can be reduced.
Intermittent fasting guidance:
12:12 gentle fasting or no intentional fasting
Emphasize hydration and electrolytes
Prioritize protein, iron-rich foods, and magnesium
Avoid: Extended or aggressive fasting. During menstruation, the body benefits more from nourishment and recovery than metabolic stress.
Follicular Phase (Days 6–14): Highest Fasting Tolerance
Hormonal environment: Estrogen rises steadily, improving insulin sensitivity, glucose utilization, and mitochondrial efficiency.
Intermittent fasting guidance:
14–16 hour fasting windows (16:8 is often well tolerated)
One 24-hour fast may be considered during this phase
For metabolically resilient women, 48–72 hour fasts may be appropriate mid-follicular
This phase generally offers the most favorable window for therapeutic fasting in menstruating women due to improved metabolic flexibility and lower progesterone influence.
Ovulatory Phase (~Day 14): Moderate Fasting Only
Hormonal environment: Estrogen peaks and luteinizing hormone surges. While energy may feel high, cortisol sensitivity increases.
Intermittent fasting guidance:
12–14 hour fasting windows
Maintain hydration and electrolyte balance
Avoid aggressive restriction
Prolonged fasting during ovulation may elevate cortisol and interfere with reproductive hormone signaling. The relationship between fasting and ovulation is highly sensitive to energy availability, making this phase particularly vulnerable to excessive restriction.
Luteal Phase (Days 15–28): Shorten Fasts to Protect Progesterone
Hormonal environment: Progesterone dominates. Caloric needs increase and insulin sensitivity is modestly reduced compared to the follicular phase.
Intermittent fasting guidance:
12:12 or 13:11 fasting windows
Include complex carbohydrates to support progesterone and serotonin
Prioritize sleep and mineral repletion
Avoid: 24-hour or multi-day fasts. Extended fasting during the luteal phase may elevate cortisol, suppress progesterone, disrupt sleep, and worsen PMS or cycle irregularity. Elevated fasting luteal phase cortisol is one of the most common reasons women experience anxiety, insomnia, or shortened cycles when restriction is applied too aggressively during this stage.
Because metabolic resilience, thyroid function, stress load, and hormone patterns vary significantly between women, intermittent fasting for women is most effective when individualized—particularly in cases of PCOS, perimenopause, thyroid dysfunction, or chronic fatigue.
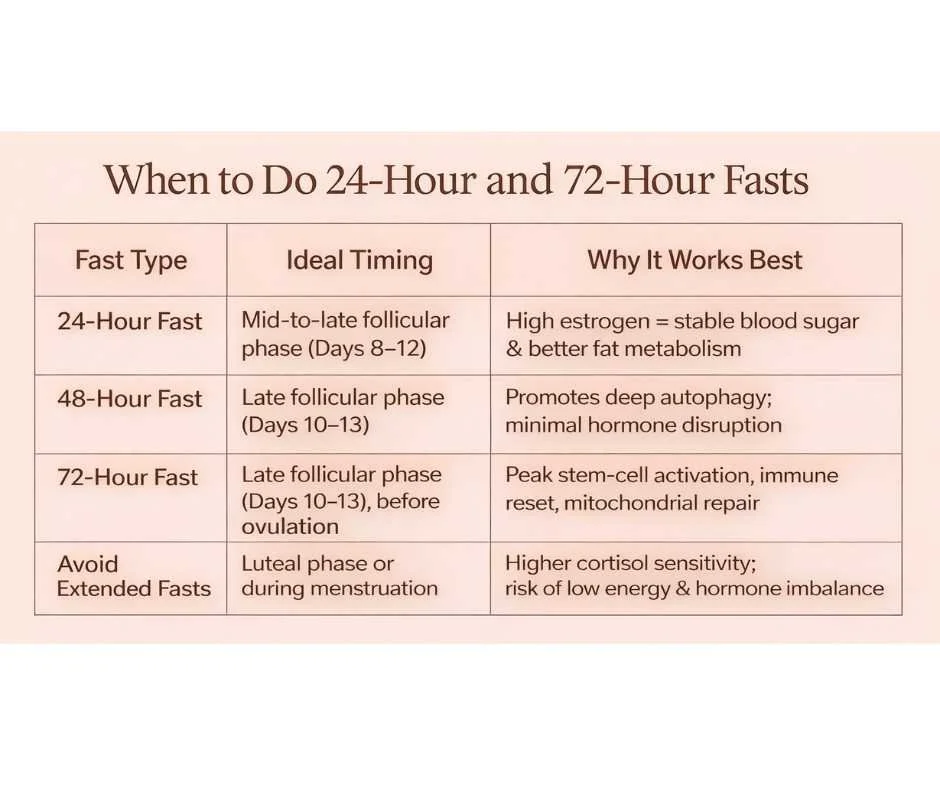
When Women Should Do 24-Hour, 48-Hour, or 72-Hour Fasts (Cycle Timing Guide)
Extended fasting for women should be timed carefully within the menstrual cycle to reduce cortisol elevation and protect progesterone stability. The follicular phase—particularly the mid-to-late follicular window—is generally the safest period for 24-hour, 48-hour, or 72-hour fasts in menstruating women.
Below is a clinically aligned breakdown of when longer fasts are typically best tolerated.
24-Hour Fast for Women: Best Timing and Hormone Considerations
Best timing: Mid-to-late follicular phase (Days 8–12)
During this window, rising estrogen supports stable blood sugar regulation, improved insulin sensitivity, and enhanced fat metabolism. Cortisol response is typically lower compared to the luteal phase.
A single 24-hour fast during this time is often well tolerated in metabolically resilient women.
48-Hour Fast for Women: Best Timing and Hormone Considerations
Best timing: Late follicular phase (Days 10–13)
Estrogen remains elevated and progesterone is still low, creating a metabolic environment more supportive of deeper autophagy with lower risk of hormone suppression.
This window reduces the likelihood of progesterone disruption that may occur if extended fasting is attempted during the luteal phase.
72-Hour Fast for Women: Best Timing and Hormone Considerations
Best timing: Late follicular phase (Days 10–13), completed before ovulation
A 72-hour fast may promote deeper autophagy, immune recalibration, and mitochondrial renewal. However, this duration should only be considered when:
Sleep is stable
Stress load is low
Thyroid function is optimized
Nutrient status is adequate
Aggressive fasting outside this window—especially in the luteal phase—may elevate cortisol and suppress progesterone.
When Women Should Avoid Extended Fasts
Avoid 24-hour or multi-day fasts during:
The luteal phase
Active menstruation
Periods of high stress or poor sleep
During these times, cortisol sensitivity is higher and caloric needs increase. Extended restriction may contribute to hormone imbalance, cycle irregularity, anxiety, or fatigue.
Pro Tip for Irregular Cycles or Perimenopause
For women with irregular cycles, perimenopause, or amenorrhea, fasting should not be based on calendar dates alone.
Instead, use biofeedback markers such as:
Energy stability
Sleep quality
Mood resilience
Hunger patterns
Body temperature trends
When hormonal rhythms are inconsistent, symptom tracking is a more reliable guide than fixed cycle days.
How Intermittent Fasting May Influence Cancer Risk in Women
Research suggests that intermittent fasting may influence biological pathways associated with long-term disease risk. For women, this conversation must remain grounded in hormonal physiology and metabolic balance rather than aggressive longevity protocols.
Rather than acting directly on cancer itself, fasting appears to influence internal conditions that may affect risk patterns over time—particularly insulin signaling, inflammation, and hormone regulation.
The broader metabolic theory of cancer and therapeutic applications are addressed separately. Here, the focus remains on how cycle-aware fasting may support overall metabolic resilience in women.
Insulin, IGF-1, and Growth Signaling
Chronically elevated insulin and IGF-1 signaling are associated with increased cellular proliferation. Intermittent fasting may help regulate these growth pathways by improving insulin sensitivity and reducing sustained metabolic overactivation.
For women, insulin regulation is especially relevant in conditions such as PCOS, obesity, and insulin resistance—each associated with altered hormone signaling.
The emphasis is metabolic balance, not aggressive restriction.
Autophagy and Cellular Housekeeping
Short-term fasting can stimulate autophagy, a regulated cellular cleanup process that removes damaged components and supports mitochondrial efficiency.
In women, this process is most appropriate during the follicular phase, when estrogen supports metabolic flexibility and stress tolerance. During the luteal phase, prolonged fasting may elevate cortisol and disrupt progesterone stability.
Cycle context matters more than duration alone.
Inflammation and Hormone-Sensitive Cancers
Chronic low-grade inflammation is associated with multiple hormone-sensitive cancers, including breast and endometrial cancers.
Intermittent fasting may reduce inflammatory signaling and improve metabolic regulation when implemented conservatively and in alignment with hormonal rhythms.
However, excessive fasting that disrupts ovulation or elevates cortisol may undermine hormone balance rather than support it.
Important Distinction: Fasting During Active Cancer Treatment
Research exploring fasting-mimicking strategies alongside chemotherapy is ongoing and not considered standard of care.
Fasting during active cancer treatment should never be self-directed and must be supervised within a comprehensive medical framework.
This article does not address therapeutic oncology protocols.
How Intermittent Fasting May Influence Cancer Risk in Women
For women, the relevance of intermittent fasting in the cancer-prevention conversation lies in:
Improving insulin sensitivity
Supporting estrogen metabolism
Reducing chronic inflammation
Maintaining metabolic flexibility
These effects are associated with lower lifetime cancer risk, but fasting is not a standalone or universal solution.
For menstruating women, fasting must remain individualized, cycle-aware, and nutritionally supported to avoid hormone suppression, excessive stress, or nutrient depletion—especially when cancer risk or hormonal imbalance is a concern.
Can Intermittent Fasting for Women Help Correct Hormone Imbalance?
Intermittent fasting for women can support hormone balance when it is cycle-synced, nutritionally supported, and matched to stress tolerance.
When fasting is aligned with the menstrual cycle and paired with adequate protein, mineral repletion, and strategic refeeding, insulin sensitivity improves and metabolic flexibility increases. These shifts influence estrogen metabolism, ovulatory signaling, progesterone production, and cortisol regulation.
However, fasting that is overly aggressive or mistimed—particularly during the luteal phase—can suppress ovulation, elevate cortisol, and worsen hormone imbalance rather than correct it.
Key hormone-supportive mechanisms include: (4)
How Intermittent Fasting Supports Estrogen Metabolism in Women
Intermittent fasting may support liver detoxification pathways, reduce inflammatory signaling, and improve blood sugar regulation—all of which contribute to healthier estrogen clearance.
Improved estrogen metabolism may benefit women experiencing:
PMS
Endometriosis
Estrogen dominance
Breast tenderness or fibrocystic breast changes
Heavy or irregular cycles
Because estrogen balance is closely linked to insulin signaling, metabolic improvements often precede symptom improvement.
Fasting, Ovulation, and Progesterone Production
The relationship between fasting and ovulation is highly dependent on energy availability and stress load. When insulin resistance and inflammation are present, strategic fasting may help restore consistent ovulatory signaling.
Ovulation is required for adequate progesterone production. Healthy progesterone supports:
Mood stability
Sleep quality
Fertility and cycle regularity
A stable luteal phase
When fasting is applied during the luteal phase without adequate caloric support, progesterone may decline. Elevated fasting luteal phase cortisol can further disrupt ovulatory stability and shorten cycles.
This is why intermittent fasting for women must be phase-aware.
Cortisol and Fasting in Women: When Stress Hormones Rise
Cortisol and fasting in women are closely linked. Short, phase-appropriate fasting windows may improve metabolic resilience and HPA-axis regulation.
However, prolonged restriction—especially during the progesterone-dominant luteal phase—can amplify cortisol output, contributing to anxiety, sleep disturbance, and irregular cycles.
Fasting for women should reduce physiological stress, not compound it.
Intermittent Fasting and Appetite Hormones (Leptin & Ghrelin)
Intermittent fasting may help recalibrate appetite signaling by improving leptin sensitivity and stabilizing ghrelin rhythms. Over time, this can reduce cravings and improve satiety regulation—particularly in women with insulin resistance or PCOS.
When implemented correctly, intermittent fasting supports hormone balance through metabolic regulation. When applied rigidly, it may suppress ovulation and increase cortisol instead.
For women with persistent hormone symptoms, thyroid dysfunction, PCOS, or cycle disruption, fasting works best within a comprehensive, hormone-supportive framework rather than as an isolated strategy.
Intermittent Fasting for Women With PCOS, Thyroid Conditions, and Perimenopause
Intermittent fasting for women with hormone dysregulation can be beneficial when it is structured, phase-aware, and metabolically appropriate. The goal is not calorie restriction—it is improved insulin sensitivity, reduced inflammatory signaling, and restored metabolic flexibility.
Fasting strategies must match hormonal context, thyroid resilience, stress load, and menstrual cycle timing.
Intermittent Fasting for Women With PCOS and Insulin Resistance
Polycystic ovary syndrome (PCOS) is strongly associated with insulin resistance, hyperinsulinemia, and androgen excess.
Strategic intermittent fasting for women with PCOS may help:
Improve insulin sensitivity
Reduce fasting insulin levels
Support healthy weight regulation
Lower androgen-related symptoms (acne, hirsutism, scalp hair thinning)
Restore ovulation and menstrual regularity
Improve fertility outcomes
Because PCOS is fundamentally a metabolic-hormonal condition, time-restricted eating may be more effective than chronic calorie restriction—provided fasting is not excessive or stress-inducing.
Cycle-synced fasting is especially important in PCOS, as aggressive restriction may elevate cortisol and disrupt ovulation.
Intermittent Fasting and Thyroid Function (Hypothyroidism and Hashimoto’s)
Fasting and thyroid health are closely linked to stress physiology and metabolic flexibility.
Short fasting windows (12–14 hours), particularly during the follicular phase, are generally best tolerated while insulin sensitivity is improving. However, prolonged or aggressive fasting—especially during the luteal phase—may increase cortisol and reduce thyroid hormone conversion in metabolically fragile individuals.
Women with hypothyroidism or Hashimoto’s should prioritize:
Stable protein intake
Adequate caloric refeeding
Luteal phase protection
Stress reduction
Fasting should enhance metabolic resilience—not compound fatigue or cold intolerance.
Intermittent Fasting in Perimenopause and Menopause
As estrogen and progesterone decline, insulin resistance, inflammation, and sleep disruption become more common.
Intermittent fasting during perimenopause may support:
Improved blood sugar regulation
Reduced inflammatory signaling
Enhanced mitochondrial efficiency
More stable energy patterns
However, cortisol sensitivity often increases during this transition. Prolonged fasting without adequate protein or mineral support may worsen sleep and stress regulation.
Short, consistent fasting windows are typically more effective than extended multi-day fasts in this population.
Postpartum Fasting (After Breastfeeding)
After pregnancy—once breastfeeding has fully ceased—short fasting windows (12–14 hours) may help restore insulin sensitivity and metabolic rhythm.
Extended fasting should be delayed until:
Sleep is stable
Nutrient status is repleted
Stress levels are controlled
Postpartum physiology is highly stress-sensitive. Cortisol and fasting in women during this period require cautious implementation.
Why Personalization Matters in Hormone Conditions
PCOS, thyroid dysfunction, perimenopause, and postpartum recovery all involve overlapping metabolic and stress-related drivers.
Intermittent fasting for women in these categories is most effective when:
Aligned with the menstrual cycle
Adjusted for luteal phase cortisol sensitivity
Matched to thyroid resilience
Integrated within a broader hormone-supportive framework
Fasting is a tool—not a standalone solution.
When Intermittent Fasting Supports Female Hormones — and When It Raises Cortisol
Intermittent fasting for women can be either therapeutic or disruptive depending on timing, stress load, and hormonal phase.
When aligned with the menstrual cycle and supported with adequate nutrition, fasting may:
Restore metabolic balance
Improve insulin and leptin signaling
Support ovulation and fertility
Reduce inflammatory hormone symptoms
Improve metabolic flexibility
However, when fasting is imposed during high-stress periods or during the luteal phase without sufficient caloric support, cortisol may rise and progesterone may decline.
The relationship between cortisol and fasting in women is phase-dependent. Follicular-phase fasting is generally better tolerated, while luteal-phase restriction may amplify stress signaling.
The goal is not rigidity—it is personalization based on hormonal biology.
At its best, intermittent fasting should reduce physiological stress, not compound it.
Who Should Avoid or Modify Intermittent Fasting (Women at Higher Hormonal Risk)
Intermittent fasting may not be appropriate—or should only be implemented under clinical supervision—if a woman:
Is pregnant or breastfeeding
Has a history of disordered eating
Is underweight or experiencing unexplained weight loss
Has uncontrolled thyroid dysfunction
Has significant adrenal stress or HPA-axis dysregulation
Is experiencing amenorrhea unrelated to menopause
Is undergoing active cancer treatment (unless medically supervised)
Has hypoglycemia or uncontrolled diabetes
In these cases, fasting may elevate cortisol, suppress ovulation, or worsen metabolic instability.
Individual hormonal context always determines suitability.
Common Intermittent Fasting Mistakes in Women That Raise Cortisol
Even well-intentioned intermittent fasting for women can backfire when applied without adequate recovery and nutrient support.
Common mistakes include:
Combining fasting with chronic stress, poor sleep, or excessive training
Ignoring warning signs such as cold extremities, anxiety, missed periods, or disrupted sleep
Skipping electrolytes or under-eating during refeeding
Applying prolonged fasting during the luteal phase
Using fasting as punishment rather than metabolic therapy
Elevated fasting luteal phase cortisol is one of the most common drivers of cycle irregularity and fatigue when restriction is misapplied.
Intermittent fasting should improve energy, clarity, and hormonal resilience—not erode them.
How We Personalize Intermittent Fasting for Women Using Advanced Hormone Testing
At Denver Sports & Holistic Medicine, intermittent fasting for women is not prescribed as a generic longevity trend. It is applied strategically—based on hormonal resilience, metabolic flexibility, thyroid function, and stress physiology.
Before increasing fasting intensity, we evaluate:
Cortisol and progesterone patterns (DUTCH testing)
Insulin dynamics and metabolic markers
Thyroid signaling and energy output
Sleep quality and recovery capacity
Glucose and ketone response when clinically indicated (GKI)
This prevents the most common mistake: using fasting to push through hormonal dysfunction rather than correcting it.
→ Functional & Integrative Medicine
When properly matched to biology, intermittent fasting may:
Improve insulin sensitivity
Support ovulatory stability
Reduce inflammatory signaling
Enhance metabolic adaptability
When layered onto stress, sleep deprivation, thyroid instability, or luteal phase vulnerability, fasting may elevate cortisol, suppress progesterone, and worsen fatigue.
The difference is not discipline—it is physiology.
If intermittent fasting has led to fatigue, anxiety, disrupted sleep, missed periods, stalled progress, or worsening hormone symptoms, that is not a sign to “try harder.” It signals the need to reassess metabolic readiness and hormonal context before increasing restriction.
→ Advanced Functional Lab Testing
You may request a free 15-minute consultation with Dr. Martina Sturm to review your health concerns and determine whether fasting is appropriate for your body at this time within a root-cause, systems-based framework.
Frequently Asked Questions About Intermittent Fasting for Women and Hormones
Is intermittent fasting bad for women’s hormones?
Intermittent fasting is not inherently harmful for women. However, fasting can disrupt hormones if it is prolonged, combined with high stress, or applied during the luteal phase without adequate caloric support. When aligned with the menstrual cycle—especially during the follicular phase—intermittent fasting for women can improve insulin sensitivity without suppressing ovulation or progesterone.
What is the best intermittent fasting schedule for women?
Most menstruating women tolerate fasting best during the follicular phase (approximately days 6–14), when estrogen supports insulin sensitivity. A 14–16 hour fasting window is often appropriate during this time. During the luteal phase, shorter windows (12–13 hours) are typically better to prevent elevated cortisol and progesterone suppression.
Should women fast during the luteal phase?
Extended fasting during the luteal phase may increase cortisol and reduce progesterone production. Many women experience anxiety, sleep disruption, or PMS when fasting aggressively during this stage. Shorter fasting windows with adequate refeeding are usually more supportive.
Can intermittent fasting stop or delay your period?
Yes. Aggressive or prolonged fasting can reduce luteinizing hormone signaling and suppress ovulation. When ovulation is disrupted, progesterone declines, which may delay or disrupt the menstrual cycle.
Does intermittent fasting raise cortisol in women?
Fasting temporarily increases cortisol as part of normal metabolic adaptation. However, prolonged fasting—especially during the luteal phase or during periods of high stress—may lead to sustained cortisol elevation in women, contributing to anxiety, insomnia, fatigue, or cycle irregularity.
Is 16:8 intermittent fasting safe for women?
For many women, 16:8 intermittent fasting is best tolerated during the follicular phase when insulin sensitivity is highest. During the luteal phase, shortening the fasting window may better protect progesterone and reduce stress hormone activation.
Can intermittent fasting help with PCOS?
Yes. Because PCOS is strongly associated with insulin resistance, intermittent fasting may improve insulin sensitivity, reduce androgen excess, support ovulation, and help regulate cycles—when implemented in a structured and stress-aware manner.
Can intermittent fasting worsen hypothyroidism?
Extended or aggressive fasting may reduce thyroid hormone conversion in women with metabolic fragility. Starting with shorter fasting windows (12–14 hours) and avoiding luteal phase restriction is often more appropriate for women with hypothyroidism or Hashimoto’s.
Can intermittent fasting cause hair loss in women?
Hair thinning may occur when fasting is combined with inadequate protein intake, iron deficiency, elevated cortisol, or excessive calorie restriction. Hair loss typically reflects nutrient depletion or chronic stress rather than intermittent fasting alone.
What are signs intermittent fasting is not working for you?
Warning signs include:
Missed or irregular periods
Cold extremities
Persistent fatigue
Anxiety or insomnia
Reduced exercise recovery
Hair thinning
These symptoms suggest cortisol elevation, progesterone suppression, or inadequate nutrient support.
What should women eat to break a fast?
Breaking a fast with protein, healthy fats, and non-starchy vegetables helps stabilize blood sugar. Avoid breaking a fast with refined carbohydrates or alcohol, which may cause glucose spikes and increase inflammatory signaling.
Still Have Questions?
If the topics above reflect ongoing symptoms or unanswered concerns, a brief conversation can help clarify whether a root-cause approach is appropriate.
Resources
BMC Women’s Health – Does Ramadan fasting have any effects on menstrual cycles?
ResearchGate – The analysis study effect of intermittent fasting on female reproductive hormones and menstrual cycle: a comprehensive systematic review
The Journal of Clinical Endocrinology & Metabolism – Short-term fasting in normal women: absence of effects on gonadotrophin secretion and the menstrual cycle
Nature Reviews Cancer – Fasting and fasting-mimicking diets for chemotherapy augmentation
Cancer Treatment Reviews – Intermittent fasting interventions to leverage metabolic and circadian mechanisms for cancer treatment and supportive care outcomes
Nutrients – The effect of time-restricted eating on insulin levels and insulin sensitivity in patients with polycystic ovarian syndrome: a systematic review
Endocrine Reviews – Endocrine and chronobiological effects of fasting in women